The Agency for Healthcare Research and Quality’s Healthcare Cost & Utilization Project has released a new infographic on hospital readmissions by diagnosis and inpatient procedure. Hospital readmission is an indicator of quality of care and is an opportunity for reducing health care costs. It can also lead to penalities against those hospitals with excessive rates.
The Agency for Healthcare Research and Quality’s Healthcare Cost & Utilization Project has released a new infographic on hospital readmissions by diagnosis and inpatient procedure. Hospital readmission is an indicator of quality of care and is an opportunity for reducing health care costs. It can also lead to penalities against those hospitals with excessive rates.
For the most common conditions and procedures, as many as one in five patients – and in some cases more than one in five – will be readmitted to U.S. hospitals within 30 days. Patients and their caregivers who are aware of these readmission rates can take steps – taking medicines as prescribed, closely following discharge instructions, etc. – to help reduce the risk of having to be readmitted.
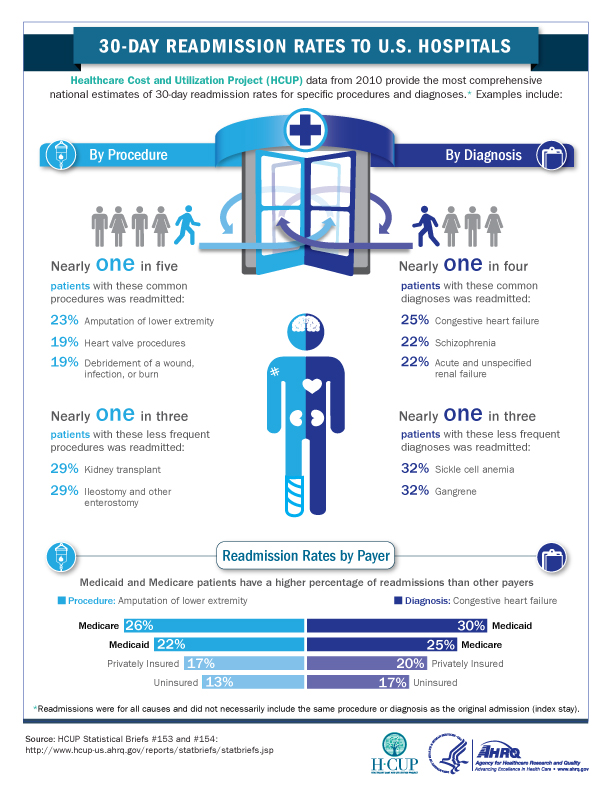
The infographic is based on two Healthcare Cost & Utilization Project (HCUP) Statistical Briefs –#153 and #154 – comprising the most comprehensive national estimates on hospital readmissions by diagnosis and inpatient procedure available to date.