The Buzz About Specialty Pharmacy
If you’ve been hearing a lot of buzz about “specialty drugs” and “specialty pharmacies” you might be wondering what exactly is being alluded to when we use these terms.
The Buzz About Specialty Pharmacy
If you’ve been hearing a lot of buzz about “specialty drugs” and “specialty pharmacies” you might be wondering what exactly is being alluded to when we use these terms. “Specialty” herein denotes prescription medications that are a step beyond run-of-the-mill medications you might be most likely to pick up at the pharmacy (like a Z-Pak for strep throat) in terms of their complexity. Either because the drugs themselves are complex and thus require careful preparation, or the administration of the drug is complex and requiring either close medical supervision or be administered by a healthcare professional at home or in a healthcare setting. Some drugs might fall into both of these categories.
Who Needs These?
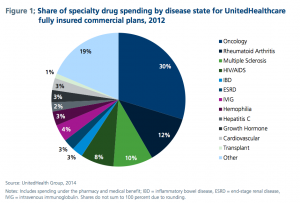
This particular type of drug is often associated with diagnoses like Rheumatoid Arthritis, Multiple Sclerosis, Hepatitis C and any number of cancers. Because these illnesses are chronic and progressive in nature, the treatments for them follow suit in terms of complexity. As you might suspect, these drugs aren’t cheap — but for the patient’s receiving them, it’s what makes the difference in their quality of life and, at times, their overall prognosis.
What Does It Mean For Payers and Providers?
What about for the payers and providers? Is the investment in specialty pharmacy accreditation and services worth it? The healthcare arena is currently being dominated by decrees of “lowering cost without compromising quality” and that’s no small feat, particularly when it’s looking like forgoing these expensive drugs may have a very negative impact on patient care — which is a compromise in quality if there ever was one.
Increased Demand Presents Financial Challenges — and Opportunities.
Whether or not either side is fully ready to embrace it, the presence of specialty pharmacies and the drugs they provide is increasing — and so too will the demand. Patients are aware now more than ever that they have options when it comes to their treatment, and with payers preparing to expand their coverage, on the patient side of things money may not always be an obstacle.
Popular drugs like Remicade, Avenox and Zenapax, which treat conditions like RA, MS and diseases where immunosuppression is needed are becoming more in demand. Pharmacies that wish to remain competitive in the market will need to gain the required education to provide and advise upon these prescriptions — or else the loss of revenue will come from patients heading to the pharmacy down the street that does carry their drug.
We’re an aging population, and many of the diseases and conditions that are front runners in drug therapy innovation afflict the demographic of patients that is rapidly dominating healthcare. These are also, consequently, the patients who are most often covered by Medicare — presenting reimbursement challenges for the providers and payers who agree to carry the specialty drugs.
Reimbursement Challenges: Will ICD-10 Help or Hinder?
On the payment side, reimbursement challenges in the form of medical billing and coding will hopefully see some resolution this year when ICD-10 finally enters the industry as our primary coding lexicon. With its high specificity and inclusion of more codes than in any previous iteration, ICD-10 may solve some of the dilemmas faced by payers when certain types of drugs are billed under these codes instead of J codes, or vice versa.
J codes typically only work for the chemical composition of the drug, not necessarily it’s manufacturer or size. J codes are assigned to a drug within 18 months after they’ve entered the market, which, when you consider how many new drugs have been approved in the last decade, means tons of new codes to deal with and many opportunities for misappropriation.
Surge of New Drug Approvals Presents Challenges
Private payers have been focused on containing costs for decades, but it’s proven to be a challenge to save money without compromising care when innovation in medicine seems to abound. One valuable distinction to make regarding specialty pharmacy drugs, however, is that while terms like “biological”, “biopharmaceuticals” and “biotech” are all used interchangeably, the types of drugs that can be classified under the umbrella of specialty pharmacy don’t always necessarily fall into one of those categories.
With all these brand new drugs entering the market, as the surge in approvals within the biotech industry over the last few years takes hold, there’s a need for pharmacies to assess whether or not they can afford to forgo accreditation as a specialty pharmacy. Perhaps it can be put off for another year, but not indefinitely; eventually the shifting payment landscape, drug innovation and patient demands will make a specialty pharmacy accreditation non-negotiable.
Don’t Get Left Behind
It would be wise to not get behind: as the number of prescriptions, patients and payers continues to increase, so will the competition. If your pharmacy is looking to nab those large contracts with payers, you can’t afford to go into the process unaccredited.
Payers are prioritizing those pharmacies who have devoted themselves to the accreditation process in part because it proves their commitment to providing top-level care to patients even as the rules continue to change. Staying relevant isn’t easy, but hopping on the proverbial bandwagon sooner rather than later will save you more than just money — it’ll save you the headache!
The post The Real Cost of Specialty Pharmacy appeared first on BHM Healthcare Solutions.