Last week CMS announced a major new initiative for Total Joint Replacement, aimed at both reducing and reconciling costs. Total joint replacements are predicted to increase at a rate of 30% to 2020. Demographics are the major driver: people are getting joint replacements at a younger age, and may have more than one in their lifetime.
Last week CMS announced a major new initiative for Total Joint Replacement, aimed at both reducing and reconciling costs. Total joint replacements are predicted to increase at a rate of 30% to 2020. Demographics are the major driver: people are getting joint replacements at a younger age, and may have more than one in their lifetime. On the one hand, more active baby boomers have put greater strain on their joints by running marathons, and on the other an overweight population is putting more strain on their joints just by walking around.
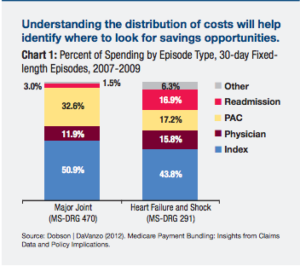
Since the demand is increasing, and the costs fluctuate wildly, up to 100% by Medicare’s estimates, the opportunities to look for costs savings and to reward based on outcomes is key. Like other bundled payment recommendations, Medicare is looking at the 90-day readmission rates and also using a carrot and stick reimbursement approach.
“Depending on the hospital’s quality and cost performance during the episode, the hospital may receive an additional payment or be required to repay Medicare for a portion of the episode costs.”
While private payers often follow Medicare, this is one area where Medicare cites that it is following a trend that has already been piloted in private scenarios, most notably with self-insured employers contracting directly with healthcare systems on fixed-price knee and hip replacements, like the deals Walmart and Lowe’s have struck directly with hospitals.
Our research has shown that a large driver of these costs is discharge setting related. While the majority of patients do better when discharged to home, they were being discharged to skilled nursing instead as a “belt and suspenders” type of back up. Discharging to the right setting, can improve patient experience and lower costs. However discharge to home requires the right type of patient tools. Patients need to have great educational materials, the ability to track their progress, and the ability to get remote help if they need it. This is something we’re passionate about at Wellpepper, and we are working with a number of leading health systems that are moving to bundled payments to help them digitize the pre and post surgical instructions and collect patient reported outcomes. We’d like to be part of the solution for both patients and providers as we move to these new models of care and reimbursement.
The Medicare proposal is open for public comment for the next 60 days. It’s over 400 pages long, so you may want to print a copy and take it for a little light beach reading.