Mental health concerns are more significant than ever. One study showed that 20% of American adults suffer from at least one mental health issue. Some of the causes of mental illnesses might surprise you.
Have you ever experienced “butterflies” in your stomach or a “gut-wrenching” feeling in tense situations? These sensations indicate that your gut and brain are interconnected.
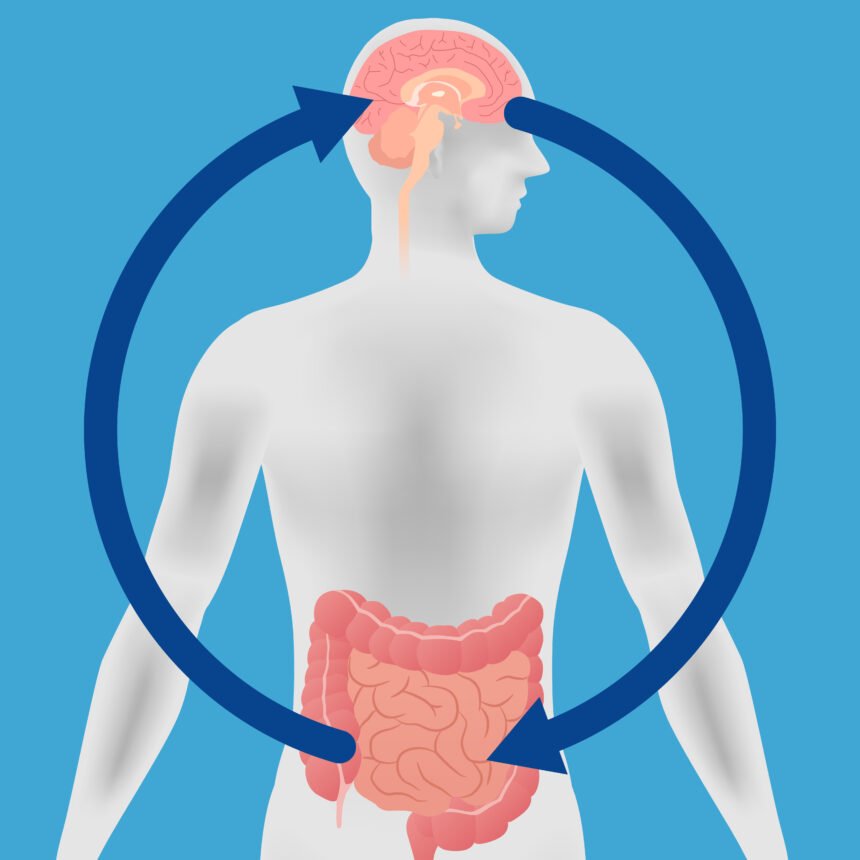
In fact, many studies have shown that your gut affects your brain health and vice versa.
This two-way communication system between your brain and gut is referred to as the gut-brain axis.
Keep reading to find out more about the gut-brain axis and what foods are good for its health.
So, let’s begin!
How are the gut and brain connected?
The gut-brain axis connects your brain and central nervous system (CNS) with the enteric nervous system (ENS) — often called the “second brain” — in your gut.
This connection is a complicated bi-directional communication network involving your immune system, nervous system (vagus nerve), and the chemical messengers (neurotransmitter) system. Your gut microbiota also plays a role in this network.
The vagus nerve
The vagus nerve is a long nerve that runs from your brain to your gut, physically connecting your digestive system to your CNS. It plays a huge role in carrying signals between the brain and gut.
Recent studies suggest that the gut microbiota, which produces substances that can affect mood, is also involved in this.
Studies on mice have shown that feeding them probiotics — live “good” gut bacteria — lowered the levels of stress hormones in their body. But after severing the vagus nerve, this no longer happened.
Other studies also suggest that a similar relationship may exist between the vagus nerve, the gut, and stress in humans.
One study found that individuals with irritable bowel syndrome (IBS) or Crohn’s disease had diminished vagus nerve function and elevated markers of stress, compared to individuals without these disorders.
Fun fact: even though the vagus nerve supplies the gut, gut contractions and secretions are regulated by the enteric nervous system without any input from the vagus. When your stomach is upset and you experience hyperactive bowel sounds, it’s because the enteric nervous system (not the vagus nerve) is in overdrive.
The gut microbiome and neurotransmitters
Neurotransmitters are chemical messengers that play a part in a variety of bodily functions. They are present in both your gut and brain and are another component of the gut-brain axis.
Your colonic bacteria can influence the production of some neurotransmitters like gamma-aminobutyric acid (GABA), dopamine, and serotonin. And all of these are vital for your emotional well-being. You especially want to be familiar with the serotonin neurotransmitters, since they have a huge impact on your mood.
In fact, our gut manufactures a huge chunk of our body’s total serotonin, and scientists believe that our gut flora helps regulate this. In the gut, serotonin plays a crucial part in processes involving digestion.
However, the changes it makes in your belly may send signals to the CNS, influencing the production of neurotransmitters there. In the CNS, serotonin plays a role in regulating sleep and mood.
Your gut microbiome also produces GABA — a neurotransmitter involved in reducing anxiety, stress, and fear. Some experts suggest that increasing “good” gut bacteria with the help of probiotics can boost the production of beneficial neurotransmitters like GABA.
The gut flora and the immune system
The immune system is your body’s natural defense system against diseases. It includes a network of cells, organs, and chemicals that work in conjunction to combat harmful viruses, fungi, and bacteria.
It’s also a huge part of the gut-brain connection. Just like your immune system can affect your gut health, your gut flora can directly influence your immune system.
In fact, a huge part of your immune system is actually located in your gut.
And although there is still a lot we don’t know about how gut bacteria affects the brain and immune system, trials have shown that the gut microbiome can influence the level of proteins known as cytokines.
These chemical substances are crucial for your inflammatory and immune response and can even influence brain function.
The connection between your gut and mental health
Even though both mental and gut health is complicated, there’s a growing amount of evidence suggesting that they can and do influence each other. Mental health disorders like anxiety and depression are often associated with gut problems like IBS.
Scientists have even identified certain colonic bacteria that may be linked with mental health conditions. A recent study found that individuals with depression had reduced amounts of two types of microbes, called Coprococcus and Dialister,in their colon.
On the other hand, participants with greater numbers of these bacteria reported better scores when asked about their quality of life.
Researchers have also found positive results when exploring the use of fecal microbiota transplants (FMT) as a treatment for mental health disorders.
FMT involves transplanting samples of feces containing bacteria from a donor’s gut flora into the patient’s gut.
Numerous trials have shown that FMT from normal donors improved symptoms in individuals with anxiety and depression.
How diet can boost mental health
There’s a lot of evidence that suggests eating healthier can boost your mental health.
One particular study found that individuals with depression experienced significant improvement in their symptoms after adjusting their diets based on a nutritionist’s recommendations.
Several other studies have also found that having better quality diets that include prebiotics — plant fibers that provide food for gut bacteria — can significantly improve your mood.
Eating fermented foods containing probiotics can also have potential mental health benefits and has been shown to reduce symptoms of anxiety.
In contrast, diets containing mostly pro-inflammatory foods like processed and fast food have been linked to depression-like symptoms.