Doctors hate the first of the year. Besides the cold weather, there are a myriad of reasons for that. In private practice one typically goes without a paycheck for two months. That’s a bit of a stressor. Increasingly more frustrating every year is all the changes from pharmacy benefit managers. Finally the physician finds the right combination of antihypertensive drugs, blood pressure is well controlled, life is good! Then the dreaded letter from the pharmacy benefits company arrives, stating that Exforge (or Metoprolol ER or…) is not covered under the patient’s insurance plan.
Doctors hate the first of the year. Besides the cold weather, there are a myriad of reasons for that. In private practice one typically goes without a paycheck for two months. That’s a bit of a stressor. Increasingly more frustrating every year is all the changes from pharmacy benefit managers. Finally the physician finds the right combination of antihypertensive drugs, blood pressure is well controlled, life is good! Then the dreaded letter from the pharmacy benefits company arrives, stating that Exforge (or Metoprolol ER or…) is not covered under the patient’s insurance plan. For some reason this year it is extended release medications on seniors’ plans that are not covered, generic no less. The elderly patient, who may be challenged in regard to compliance, now must take his or her medicine two or three times a day instead of just once. No problem, I’m sure the insurance company will send out a nurse to make certain that the patient takes all medications properly. No wait, the nurse is busy sending the patient to the emergency room for a hangnail because she’s worried that pain in the left arm is cardiac. But I digress.
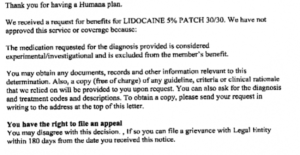
This week a new level of denial has been breached. Now medications are deemed “experimental”. Somehow pharmacy benefit managers have confused off-label with experimental. Why would they do that? Simple: off-label use isn’t excluded on a patient’s insurance but experimental is. In one particular case my patient has a progressive debilitating neurologic disease that is causing pain. The patient already has issues with constipation due to an inability to be mobile so narcotics are not a good option, not to mention that he does not want to be dependent on narcotics for this pain. Amazingly this “experimental” medication was doing a good job of managing the pain for the last year or so.
Not only is the denial of this medication arbitrary and cruel, it is unethical. Off label use of medications is an accepted and necessary treatment choice, particularly with pain, where avoiding narcotics is important for patient quality-of-life and many off-label use of medications is well-studied but not in the drug’s package insert since the medication has long been generic. In the meantime the patient asks ME how to deal with the issue. I recommended that they call their insurance company to begin an appeal process. Frankly a good lawyer might be a good idea as well.