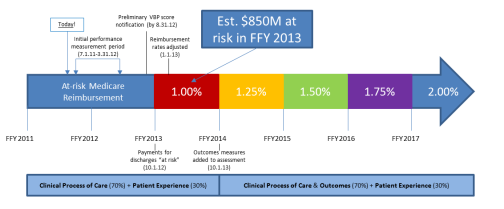
Poised at the nexus of Supreme Court oral arguments for health care reform constitutionality and the close of the Centers for Medicare and Medicaid Services (CMS) Hospital Value-Based Purchasing (HVBP) nine month performance period (July 2011-March 2012), hospitals eagerly anticipate news regarding their FY2013 Medicare reimbursement. Beginning October 2012, CMS will reduce base operating diagnosis-related group (DRG) payment to all hospitals reimbursed under the inpatient prospective payment system (IPPS) model by 1 percent, with the amount gradually increasing to 2 percent by FY 2017. Monies withheld will be used to create an incentive fund for future hospital performance based payment relative to identified domains of quality measures. Final determination of payment from the 1 percent withholding will be calculated as a linear function based on all participating entities, meaning that organizations must demonstrate continuous quality improvement in order not to fall behind their peers.
As outlined in the FY 2013HVBP final rule, an overall performance score will be calculated by assessing achievement and improvement for an institution’s Clinical Process of Care Measures and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) patient survey feedback. In determining the final score, CMS will weigh the HCAHPS results at 30 percent and the Clinical Care Core Measures results at 70 percent.
For each of the 17 measures (12 identified for FY2013 shown below) included under the Clinical Process of Care Measures, CMS will use hospital data to calculate a performance score ranging from 0 to 10. A hospital earns an achievement score based on how well it did relative to a lower threshold and upper benchmark (generally 1.0 or 100%) calculated from all hospitals’ previous baseline scores, and an improvement score based on whether it beat its own performance during the baseline period. CMS uses the higher of these two scores for its official tally. In theory, a hospital could receive all 10 points if it beats the achievement benchmark, or 0 if it fails to meet the achievement threshold or better its own previous score.
| Measure ID | Clinical Process of Care Measure Description | Threshold |
| AMI-7a | Fibrinolytic Therapy Received Within 30 Minutes of Hospital Arrival | 0.6548 |
| AMI-8a | Primary PCI Received Within 90 Minutes of Hospital Arrival | 0.9186 |
| HF-1 | Discharge Instructions | 0.9077 |
| PN-3b | Blood Cultures Performed in the Emergency Department Prior to Antibiotic Received in Hospital | 0.9643 |
| PN-6 | Initial Antibiotic Selection for CAP in Immunocompetent Patient | 0.9277 |
| SCIP-Inf-1 | Prophylactic Antibiotic Received Within One Hour Prior to Surgical Incision | 0.9735 |
| SCIP-Inf-2 | Prophylactic Antibiotic Selection for Surgical Patients | 0.9766 |
| SCIP-Inf-3 | Prophylactic Antibiotics Discontinued Within 24 Hours After Surgery End Time | 0.9507 |
| SCIP-Inf-4 | Cardiac Surgery Patients with Controlled 6AM Postoperative Serum Glucose | 0.9428 |
| SCIP-VTE1 | Surgery Patients with Recommended Venous Thromboembolism Prophylaxis Ordered | 0.95 |
| SCIP-VTE2 | Surgery Patients Receiving VTP w/I 24Hours Prior to Surgery to 24 Hours After Surgery | 0.9307 |
| SCIP-Card-2 | Surgery Patients on a Beta Blocker Prior to Arrival Receiving a BB During the Perioperative Period | 0.9399 |
Scoring remains relatively the same for the eight measures based on the HCAHPS patient surveys. Hospitals, however, also can earn up to 20 consistency points based on how well their single lowest score stacks up to the competition. Hospitals will receive a percentage grade based on how many points they scored out of the possible total. CMS will post all scores on its Hospital Compare site and use the final performance score to determine the value-based incentive payment.
| Domain | Question | Min | 50th % | Benchmk |
| Nursing | Nurse courtesy and respect | 38.98 | 75.18 | 84.7 |
| Communication | Nurse listens carefully | |||
| Nurse explanations are clear | ||||
| Doctor | Doctor courtesy and respect | 51.51 | 79.42 | 88.95 |
| Communication | Doctor listens carefully | |||
| Doctor explanations are clear | ||||
| Staff | Did you need help in getting to bathroom? | 30.25 | 61.82 | 77.69 |
| Responsiveness | Staff helped with bathroom needs | |||
| Call button answered | ||||
| Pain | Did you need medicine for pain? | 34.76 | 68.75 | 77.9 |
| Management | Pain well controlled | |||
| Staff helped patient with pain | ||||
| Medication | Were you given any new meds? | 29.27 | 59.28 | 70.42 |
| Instructions | Staff explained medicine | |||
| Staff clearly described side effects | ||||
| Discharge | Did you go to a home or another facility? | 50.47 | 81.93 | 89.09 |
| Information | Staff discussed help needed post discharge? | |||
| Written symptom/health info provided | ||||
| Cleanliness and Quietness | Area around room quiet at night | 36.88 | 62.8 | 77.64 |
| Hospital | Room and bathroom kept clean | |||
| Overall Rating | Hospital rating question | 29.32 | 66.02 | 82.52 |
While CMS’ Hospital Value-Based Purchasing Final Rule refers to Medicare patients only, private payers are quickly advancing towards a quality based reimbursement model as well. As the bar continues to be raised in pursuit of improved quality and better value, how will your organization prepare for this challenge? With less time to address the much more speculative HCHAPHS scores, does this provide the greatest area for improvement? Since many enterprising organizations are currently engaged in this process, will innovative technology coupled with collaborative continuous quality improvement keep your institution in the race?
Principle Healthcare Associates is an expert resource and dedicated advocate for Nurse Practitioner, Physician Assistant, Physician and Healthcare Executive job seekers. With many years of recruiting experience, we deliver strategies to help clients identify diamonds in the rough and candidates that stand head and shoulders above the competition.
*Graphic courtesy of Triple Tree Research