A “medical futurist” was telling the hospital board how that in the future you will have an avatar for a doctor, or a hologram – like Star Trek. This person will have access to all your medical information, and be able to tell you what modifications to make to keep you out of trouble in the next year.
To this, Katherine Gottlieb, President of South Central Foundation responded, ” We already have that, but instead of an avatar we use a real person.”
A hologram will never replace a real doctor
South Central Foundation, the primary care provider for 50,000 Alaska Natives (indigenous Alaskans, or Indians as some of you may call us) won the Malcolm Baldridge award in 2011 for Health Care. The key to the system is it is built on a relationships. Healthcare improves if you have a relationship with your doctor.
What they have done in health care is remarkable – winning awards, having many healthcare systems coming to learn their model – but here is my story:
For a doctor to see a doctor they really have to be sick
It started with a bit of congestion for the nose, and the drip made a little bit of a sore throat. Thought it was a cold for a bit then realized, it was allergies so I started to take the antihistamine, Zyrtec. During the day my nose was running, voice was hoarse, and eyes were itching. I started to cough, violently – and realized that the pollen had now reacted with my reactive airway disease (asthma) and I needed an inhaler
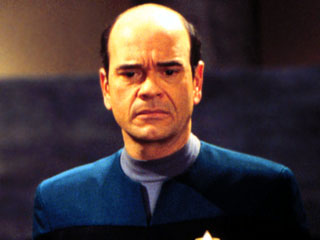
Dr. Steve Tierney – my doctor, a real doctor not an avatar or hologram
The symptoms became worse. If I stayed inside it was tolerable. But going outside made every symptom worse. Every breath I took outside felt as if I was sandblasting my nose, mouth, eyes, sinus, and lungs. My sleep was interrupted multiple times a night by waking up with fits of coughing. I had to sleep on four pillows just to get some rest with a cough drop between my teeth and cheek, hoping not to choke on it.
It was from this that I started to look up allergists in Phoenix. But there wasn’t time to get an appointment, as I was leaving town in a day.
Looking forward to the meetings in Anchorage, because it meant a break away from allergy season in Phoenix. As soon as I stepped off the plane in Anchorage I took a big gulp of air. The air didn’t hurt, it was fresh, cool. But my lungs, still inflamed from my body fighting the pollen, had yet to heal. That night, slept on three pillows. Couldn’t even get to sleep without coughing until 1:30 am, and woke up every hour.
The Best Health Care System
It struck me as I woke up in a coughing fit that I was sitting on the board of the greatest health care system in the United States, maybe the world. They were known for same-day appointments, keeping people out of the hospital, and had some great doctors. Why not contact one of the doctors here?
I knew Steve Tierney for years. Besides being one of the primary care doctors who had taken care of a number of my friends, I liked him. His wife is also a vice president of South Central, she had a good sense of humor and had put up with my rantings as a board member in good cheer.
Email your doctor?
Sometime in the early morning I sent him an email with the subject “Maybe this Dr needs a dr.” and described by symptoms and asked if I might need some medicine. I was hesitant, concerned, wondered if I would get brushed off, ignored, told to call for an appointment. I got ready to head to the meeting.
Five minutes before the meeting started I received a text from Steve, I told him where I was he said he would be there in five minutes. Still worried – every doctor does, we don’t just have asthma we have lung cancer. For me a special worry, since I saw my brother die from lung cancer a few years before. Coughing and unable to catch his breath, as I was doing. Or perhaps it could be I had heart failure, and what I thought was asthma keeping me up was simply my heart finally rebelling against years of eating red meat (if only I had stayed a vegetarian). If you think you know a hypochondriac, look at your physician, they are the worse – we know everything that can happen, and it can happen to us. We don’t get headaches, we get brain tumors — untreated and they go away. We don’t have plaque on our teeth causing gum irritation and need a dental cleaning, we get leukemia – untreated and it goes away. It starts in medical school with every disease we hear about we personalize it and get the disease. When, as a second year medical student, I was hearing about how overactive adrenal glands can cause a belly, I went to the professor and said I had this disease, and that explained my midline — in his thick German accent he told me, “Yes, you do have an overactive gland causing that. ” Relieved that he understood me, until he finished the thought, “You have an overactive mouth gland, eat less and move more.”
The hypochondria of disease never leaves a doctor, and at this point I wasn’t sure if I should arrange for hospice because of heart failure or lung cancer, but the doctor was coming and I was going to get my sentence.
Steve walked up with a smile and re-assuring tone. He asked a few questions, and paid very close attention to the answers. Told me he wanted to prescribe some prednisone to cool down the inflammation, add another anti-histamine, and an oral steroid, and get me a new inhaler (since my inhaler was about five years old).
Enrolling in the Greatest Health Care System
He said he could call in the prescriptions to a local pharmacy, or, if I wanted, I could enroll as a patient. Why not enroll? He arranged to send up the two page form, it took me two minutes to fill out. My wife sent the appropriate id card, they took a copy of my divers license and insurance card.
An hour later four prescriptions were delivered to me, at no cost, no co-pay, no deductible.
Two days later I was much improved.
Here is the thing: I have insurance and can go to any hospital, any healthcare system in the world. As a physician in Phoenix I could easily get into Mayo Clinic, or any clinic with a phone call or two. Here is the difference:
SouthCentral is built on relationships. I got to see that relationship first hand. You are not a “patient” at SouthCentral, you are a “customer-owner.”
My system- my healthcare system. Built on relationships.
And, Dr. Tierney, I can never thank you enough – not only did you treat my asthma and allergies – but cured the lung cancer and heart disease!
A few notes:
SouthCentral reported a reduction in children going to the emergency room for asthma because they see the customer-owners the same day.
SouthCentral has the lowest cost of healthcare per capita
Same day ability to see patients in the primary care center.
Fast Track in the ER
No co-pay or deductible for insurance
No out-of-pocket expense
Highlights
Southcentral Foundation’s unique Nuka System of Care is a relationship-based health care delivery system. Nuka’s organizational strategies and processes; medical, behavioral, dental and traditional practices; and supporting infrastructure work in partnership with the Native Community to support physical, mental, emotional, and spiritual wellness. The system is owned, managed, directed, designed, and driven by Alaska Native people.
In 2010, SCF achieved the highest level of Patient Centered Medical Home™ recognition from the National Committee on Quality Assurance (NCQA) for creating a strong primary care system that engages customer-owners and offers a broad range of preventive services and treatment.
Overall, SCF has achieved significant improvements in a number of key areas, including same-day access to care which has led to a 50 percent decrease in costly emergency room and urgent care visits; a decrease in specialty care by about 65 percent; a decrease in primary care visits by 20 percent; and a decrease in hospital admissions by 53 percent.
Overall staff turnover has decreased from 37 percent in 2008 to 17 percent in 2011. Turnover rates for Alaska Native and American Indian employees (who make up 53 percent of the SCF workforce) for the same period decreased from 29 percent to 15 percent.
Southcentral Foundation (SCF) is a nonprofit health care organization established in 1982 to improve the health and social conditions of Alaska Native and American Indian people, enhance culture, and empower individuals and families to take charge of their lives. SCF provides a wide range of programs to address physical, mental, emotional, and spiritual wellness for about 55,000 Alaska Native and American Indian people. Of these, 45,000 reside in the Anchorage area and 10,000 live in 55 remote villages accessible only by plane. SCF’s total coverage area, known as the Anchorage Service Unit (ASU), spans some 100,000 square miles. The ASU is served by a network of 24 health care facilities, including SCF’s two primary care centers (Anchorage and Wasilla) and two clinics (Iliamna and McGrath), and 16 subregional centers that SCF partners with to provide regional support. SCF employs 1,487 people—of which 53 percent are Alaska Natives or American Indians—and reported $201.3 million in revenues in 2010.
‘Nuka’ Means Strength in Health Care
- Southcentral Foundation’s unique health care delivery system, the Nuka System of Care, brings together organizational strategies and processes; medical, behavioral, dental, and traditional practices; and infrastructure that work together to support wellness. “Nuka” is an Alaska Native name given to strong, giant structures and living things. The system is owned, managed, directed, designed, and driven by Alaska Native people, referred to as “customer-owners.”
- The Nuka System of Care is based on four principles: (1) customers drive everything, (2) customers must know and trust the health care team, (3) customers should face no barriers in seeking care, and (4) employees and supporting facilities are vital to success.
- In 2010, SCF achieved the highest level of Patient Centered Medical Home™ recognition from the National Committee on Quality Assurance (NCQA) for creating a strong primary care system that engages customer-owners and offers a broad range of preventive services and treatment.
Superior Performance to Improve Wellness
- Overall, SCF has achieved significant improvements in a number of key areas, including same-day access to care, which has led to a 50 percent decrease in costly emergency room and urgent care visits; a decrease in specialty care by about 65 percent; a decrease in primary care visits by 36 percent; and a decrease in hospital admissions by 53 percent.
- Same-day access is achieved through a system that allows customer-owners to arrange to see their primary care provider on the same day as long they call by 4 p.m. and arrive by 4:30 p.m. This ensures that 70 to 80 percent of appointment slots are open at the start of each day.
- Among the family wellness objectives set forth by SCF is a strong effort to reduce the incidence and improve the management of diabetes, a condition experienced by Alaska Native and American Indian people at twice the national rate. Since 2009, performance levels for diabetes care exceed the 90th percentile of the Healthcare Effectiveness Data and Information Set (HEDIS), a tool used by the majority of America’s health plans to measure performance on important dimensions of care and service. HEDIS measures different areas of diabetes prevention, diagnosis, and treatment such as ensuring that diabetic patients receive their annual HBA1c screening (a test that measures blood sugar levels over a period of three months), and treating diabetic nephropathy (kidney disease and damage).
- SCF manages performance data through a state-of-the-art database dubbed DataMall. Balanced Scorecard, operational, voice-of-the-customer, and clinical information is collected, aggregated, trended, and segmented by the system, which then makes it readily available to managers, clinicians, customer-owners, and employees. Information in DataMall is used for tracking performance, driving improvement and innovation, and sharing best practices.
- SCF senior leaders have created an environment for organizational learning, performance improvement, and the accomplishment of strategic objectives through the use of an internal functional committee structure. This structure incorporates quality assurance and performance improvement committees, external benchmarking, and leadership development into corporate processes.
A Modern Alaska Native Tradition: Satisfaction
- In a 2010 survey, SCF received an overall customer satisfaction rating of approximately 91 percent.
- Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys ask consumers to report on and evaluate their experiences with health care. Using CAHPS TopBox scores (which display the percent of respondents reporting the most positive response for a composite, rating, or question item) as a benchmark, SCF’s overall satisfaction rating was 73.3 percent in 2011. This significantly exceeds the CAHPS TopBox benchmark of 46 percent.
- Overall staff turnover has decreased from 37 percent in 2008 to 17 percent in 2011. Turnover rates for Alaska Native and American Indian employees (who make up 53 percent of the SCF workforce) for the same period decreased from 29 percent to 15 percent.
- SCF administers the Morehead Associates’ Workforce Commitment Survey annually to all employees. The survey uses a five-point scale to measure employee response to a number of questions about the workplace. From 2005 to 2009, SCF improved its satisfaction scores for benefits (from 3.69 to 3.89), balancing work and personal life (from 3.67 to 3.87), interest in employee health and wellness (from 3.58 to 4.02) and management’s concern with employee safety (from 3.88 to 4.30).
Increasing Revenue While Cutting Costs
- SCF’s total revenue has consistently increased from $120.2 million in 2003 to $201.3 million in 2010, exceeding the Medical Group Management Association (MGMA) 90th percentile in 2010. Third-party payer revenue increased from $7.4 million to $17.9 million in the same time period, also exceeding the MGMA 90th percentile in 2010.
- SCF’s per capita expenditures percentage change has been lower than the MGMA benchmark since 2005. Even with phenomenal growth in the last decade, the per capita cost remains lower than the percentage increase in national health care or MGMA multi-specialty practice spending.
- Overhead expenses have decreased in recent years, meeting SCF’s target of 15 percent in 2010 and 2011.