- The percentage of non-elderly people with employer-sponsored insurance declined 10.2 percentage points from 69.7% to 59.5% over the study period while pubic coverage increased 3.1 percentage points.
- While most states saw “significant declines” in employer-sponsored insurance coverage, the range was wide—from New Hampshire (73.8% coverage) to New Mexico (48.0% coverage).
- Employer-sponsored insurance coverage varied by income. It fell less (2.8%) for high-income groups (400% federal poverty level [FLP] or above) than for those with lower incomes (200& FPL or below) where the fall was 10.1%.
- Nationally, the percentage of private-sector firms offering employer-sponsored insurance fell from 58.9% to 52.4% (although the percentage of workers eligible for coverage at firms that offered employer-sponsored insurance held steady). The take-up rate also fell from 81.8 percent to 76.3 percent. Small firms offering coverage declined (67.7% to 56.3%) while at large firms it remained essentially unchanged.
- Single-person premium costs doubled ($2,490 to $5,081); family premiums rose 125 percent ($6,415 to $14,447); employee contributions increased (17.5% to 20.8% of the total premium).
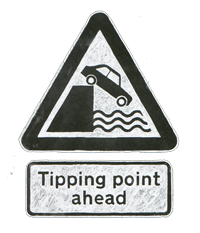
In short, less than 60% of adults who are employed full-time now have employer-backed group health insurance coverage. My response in the G+ thread? HALLELUJAH. The prospect of losing group health insurance scares the pants off of those who still have that coverage. What I say to those who are currently pants-ing themselves in fear of losing their coverage is: keep calm, and carry on. There is a path to group coverage – even keeping the coverage you now have – if your employer wants an exit strategy on paying for health insurance for their employees. I’m not an HR expert. I’m not in the insurance industry. I’m a journalist and writer who has built up, over a couple of decades, a wealth of both research and anecdotal experience in buying healthcare, buying health insurance, and being a member of the great unwashed, um, un-insured. When it comes to healthcare and the purchasing of same, I’ve been there, done that, have the t-shirts/knife scars/stories to prove it.
Employer chooses give-employer-backed-the-Heisman option
- Smart employers will raise this issue in a conversation with their employees, not as a done deal. This will take at least 3-6 months of discussion, team meetings, all-hands meetings, and will likely include at least a few opportunities for people to gnash their teeth and rend their garments, because this will scare the pants off of them. That’s the first rent garment: the pants.
- The idea needs to be shared as an ultimate win for the employees (it is), not as “we don’t wanna pay any more” whinging.
- Your HR and marketing teams will be invaluable resources here. Work with them ahead of making any announcements about the plan to create online and handout resources for your employees that will help them walk themselves through the plan and process. All of these resources should have a solid answer to any employee’s “what’s in it for me?” questions.
- UPDATE: [added as a result of a conversation on Facebook] Employers need to look at what they’re paying in insurance premiums for their crew, and adjust salaries to help defray the premium costs that will, as a result of this decision/process, directly out of their employee’s pockets. This should be (a) obvious and (b) freakin’ obvious.
Selling the roll-your-own option to employees
- If this is your first trip down the change-management path (if it is, how long have you been in business?? really??), hire a change management expert to work with you on this. If it’s not your first change-management rodeo, you already know you’ll be doing this.
- Work with that change management team and your health benefits broker – who will continue to be a critical player and your BFF throughout and after this process – to build a plan that will, over 6-12 months, shift from “company pays” to “individual pays” on health insurance premiums.
- Your benefits broker will be the expert on maintaining the existence of “the group” under the new regime. Given that the same people are being covered, there should not be a big uptick in premium cost. If there is, your broker can horse-trade to keep premiums as flat as possible.
- I strongly recommend shifting, over the two years that follow “we’re changing this whole thing” and the implementation of same, to a high-deductible health coverage plan that includes a health savings account (HSA) if you have not already done this.
- Here is where things get interesting (really) – you’re going to have to spend some money short-term to save money long-term. The money you’ll spend is to fully fund each and every employee’s HSA to the extend of their annual deductible. If their annual deductible is $5,000, you put $5,000 in their HSA. Yes, I can hear the screaming, but here’s the thing: you’ll only have to do that once. Once you’ve fully funded everyone’s first year’s deductible, they’ll make contributions (via payroll, pre-tax) each pay period to their HSAs. The amount of that contribution will be their choice.
- Premiums are paid by your employees, not by you. Your payroll deductions system will be funneling regular employee contributions to their HSAs. You can be a mensch and match HSA contributions if you want. Your payroll deductions system can also help your employees pay their health insurance premiums – your broker can advise you on how to set that up in the planning phase of setting up your Brave New Health Insurance World.
- You’ll be devoting a bit of HR time to helping your employees and your broker work together on managing the group plan, but you will no longer be footing the bill for health insurance. As said in the last bullet, you can be a mensch and kick in on their HSAs – that’s now a true benefit of working for you, right?
- Worried about the Obamacare penalties for not offering health insurance coverage to your crew? (Here’s a handy chart from the Kaiser Family Foundation that outlines those penalties.)Don’t, and here’s why: if you have fewer than 50 employees, you’re off the hook. If you have more than 50 employees, that penalty is $2,000/employee. Annual health insurance premiums currently average around $5,000 for individuals and $14,000 for family coverage. I’m not a mathematician, but all I need are basic arithmetic to know that $2,000 saves you between $3,000 and $12,000 per employee in that first year.
Important considerations and actions
- HSAs are currently not allowed to pay insurance premiums. Get your state and federal representatives to start looking at changing those laws.
- Join those calling on state insurance commissions to make health insurance products more 50-state (like Geico and Allstate) rather than the state-by-state hodge-podge that currently exists.
That’s my story, and I’m stickin’ to it. Got an opinion you’d like to share? Want to beat me up in the comments? Go for it.