Health Innovators Collaborative, University of WA Bioengineering
Dr. Jurgen Unützer, Chair of UW Psychiatry and Behavioral Sciences
Health Innovators Collaborative, University of WA Bioengineering
Dr. Jurgen Unützer, Chair of UW Psychiatry and Behavioral Sciences
The Health Innovators Collaborative seminar that I attend last week by Dr. Unutzer gave me an emotional whirlwind, which is ironic because the subject was mental health. That afternoon I innocently put my boots on and galloped down to the university in my VW Beetle and waited for the seminar to begin by eating an apple in the front row. I had no idea what was in store for me in the next 60 minutes or so. I would have cowardly slumped down into my chair if this was a talk taking place outside of Washington… because I am so ashamed about how we brush our mental illness folks under the rug. My jaw almost dropped in shock; we are ranked 48 out of 51 to have the correct resources available for our mentally ill with only 20 psychiatrists in Rural Washington. Dr. Unutzer argued that we spend more money on preventing auto accidents and homicide, when the rate of suicide is much higher- there is a suicide every 15 minutes in our country and 2-3 a day in Washington.
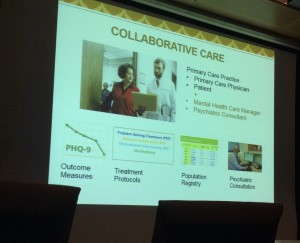
After giving us such somber news he talked at great lengths about ‘working smarter’ in order to close the gap of inadequate mental health professionals. One of the largest treatment trials for depression, Improving Mood–Promoting Access to Collaborative Treatment (IMPACT) was spearheaded by Dr. Unutzer and his colleagues. They designed IMPACT to function in two ways; “The patient’s primary care physician works with a mental health care manager (can be a mental health nurse, social worker etc.) to develop and implement a treatment and the mental health care manager and primary care provider consult with psychiatrist to change treatment plans if patients do not improve.” The IMPACT study was started over 15 years ago when the use of EMRs and video conferencing were just starting to become ‘mainstream’. Therefore in a way this study was the forerunner in utilizing a multi-based ‘high tech’ mental health patient care platform; population registry/database (tracking tool of patients PHI, treatments, etc.) psychiatric consultation (video), treatment protocols and outcome measures (I feel I am writing about Wellpepper!). The video consultation takes place between the patient and a remote psychiatrist typically after treatments protocols are administered in the primary cares office with little or no patient improvement. This is imperative especially in Washington where half of the counties don’t have a single psychiatrist or psychologist.
There is a great JAMA article written on the outcomes of the IMPACT program (I am proud to say I did my homework on the positive slides presented and not the slippery slides) that really nails out the particulars in the normal scientific journal fashion. As always I shot to the bottom of such article for the ‘results and conclusions’ because I knew this one was going to be great, I had a sneak peak last Wednesday. After a year 45% of the 1801 patients studied had a 50% or greater reduction in depressive symptoms from baseline compared with 19% of usual care participants! Furthermore this study reduced healthcare costs; $6.50 saved for every $1 invested, with the most being saved in inpatient medical and pharmacy costs. In conclusion having a system that provides population based care, that is patient centered, has target treatment solutions, and is evidence based leads to more efficient modes of getting a patient in and out the door with positive results.
I exhaled what a clever man you are Dr. Unutzer to present your slides in such an order, from negative/scary to positive/uplifting, it’s almost like you are a psychiatrist and now how the mind works, oh wait you are!! Thank you for a wonderful talk, it was superb and always nice to learn something new!
Next seminar is “Bad Language, Worse Outcomes” with Jeremy Stone, MD MBA on November 3.