According to an issue brief by Deloitte Center for Health Solutions, Value-based pricing for pharmaceuticals: Implications of the shift from volume to value, a shift in risk is occurring in the pharma industry as a result of healthcare legislation, culminating with the Affordable Care Act (ACA). The ACA was designed to increase quality while decreasing healthcare spending. All of the provisions, including value-based purchasing, are designed to achieve both of these goals.
Value-based purchasing is not actually a new concept. CMS has been piloting different initiatives since 2003 and has experienced great success. Early results obtained for the first three years with the Physician Group Practice Demonstration showed $25.3 million in Medicare savings as well as elevated composite quality scores. The ACA provisions related to value-based purchasing became effective in 2013 with the following goals:
- Shift payment/reimbursement from volume to value and from quantity to quality
- Require care coordination across many different delivery systems such as hospitals and primary care
- Be dynamic
- Build on the work and successes achieved through organizations such as CMS
- Shift risk from nearly 100% payer assumed to more of a shared risk between payers and providers, providing more accountability to providers
CMS has also created steps along the way as providers shift from fee-for-service to fee-for-value such as Accountable Care Organizations (ACOs) , comparative effectiveness research, evidence-based medicine, and bundled payments. These delivery systems begin the risk shifting process, the collaborative efforts, and the emphasis on quality/value, and a method for reducing healthcare spending.
What is Value in Terms of Value-Based Purchasing?
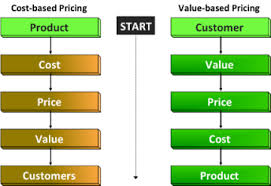
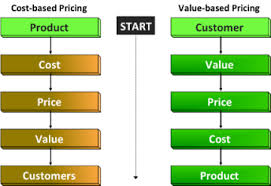
Value is one of those relative terms that have different meanings to different individuals or groups. In general, we have the following definitions so the first step in any value based purchasing agreement is mutually deciding on what value is.
- Payers think of value in terms of cost effectiveness
- Facilities think of value in terms of impact to the budget while also emphasizing patient outcomes
- Providers are concerned with budgetary impact as well as revenue generation
Trends Leading up to Value-Based Purchasing for Pharma
- Form the payer side, payers are trying to control costs through different means such as utilization management, network design, and benefit design
- Consumer out-of-pocket expenses are on the rise and generic pharmaceuticals are gaining in popularity
- Payers are gaining bargaining power with pharmaceutical companies in terms of price
- Healthcare Reform is focusing heavily upon reimbursement methodologies
- Shift in the marketplace from a consumer/pharmacy market to an institutional or facilty-based market
- Medical facilities are moving toward value-based purchasing
- Shift from reimbursement for service by individual provider to reimbursement for an episode of care across more than one provider
Things to Consider with Value-Based Purchasing:
- Which value attributes are to be collected?
- How will value attributes be measured? (weighted/non-weighted)
- When will the value attributes be measured? (initially and incrementally)
- What will the sample size be?
- How will you consumers who take more than one prescription /day?
- How will the data be collected?
- Who will collect the data? (pharma or payer)
- How do you know the results are valid and reliable?
- How will you handle the variation in regulation among states as well as changes to federal regulation such as the ACA?
- How are you defining value? (value as compared to what)
- What will be the price and how is that determined?
- How will pharma align with payers?
- Who will bear the cost for EHR/HIE implementation?