The adoption curve for virtual healthcare and telehealth has been mighty steep. In the real world, a large slice of the American public expects everyday living to be “digitally-enabled”…faster, quicker and easier. But healthcare delivery has been a sluggish exception. This picture is changing, and with it, your healthcare marketing and advertising plans may be adopting a theme. Two significant factors—patient convenience and growing provider reimbursement—are powering a fresh upswing in this trend. Patients expect convenience in service… On one hand, patients clearly want the convenience of virtual healthcare. A recent study published by Xerox reaffirms the concept that “the majority of Americans are open to and excited about virtual health. Convenience was cited as the top benefit (59 percent), followed by potential cost savings (40 percent) and the ability to see or communicate with healthcare professionals for minor ailments and the option to easily refill prescriptions – both 35 percent.” Xerox wants to help answer these consumer needs, recently launching Virtual Health Solutions. But, despite patient expectations and demand, the obstacles to delivering virtual healthcare are well known. The same Xerox survey identified the top five patient concerns:
“My insurance won’t cover it (43%); “My data and information won’t be secure (37%); “I won’t have the same personal relationship with my provider (35%); Connection issues (such as Internet/Wi-Fi/phone) (34%); and I won’t have access to my regular physicians (30%).”
Physician reimbursement is coming online…
While the number of US telehealth users is growing, the picture for physician reimbursement is slowing finding a consistent plan. “The most predominant reimbursed form of telehealth is live video,” according to HIS Technology research. “The District of Columbia and 47 states provided reimbursement for live video in Medicaid fee-for-service last year. Nine states reimburse for store and forward telemedicine, and sixteen states offer reimbursement for remote patient monitoring (RPM), remaining static from last year.”
You don’t need an appointment. Just a connection.
Two recently launched health system programs that bring telemedicine to the patient are Cleveland Clinic’s Express Care Online, and UPMC’s AnywhereCare program. EXPRESS CARE ONLINE by Cleveland Clinic stresses patient convenience adult and pediatric patients. “When you need to find care, let us bring a healthcare provider to you. From your phone, tablet or computer, at home or work, now it’s never been easier for patients to access the expertise of Express Care Online. Connect within minutes. 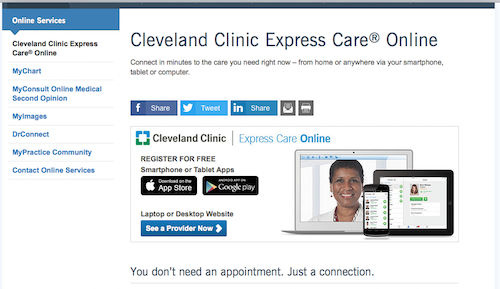
The future of virtual health…
The marketing lesson in these two examples is how healthcare providers are adapting delivery to patient preferences. What’s more, healthcare consumers are increasingly empowered in their decision process. Accordingly, healthcare marketing will continue to emphasize convenient options.