“It is far more important to know what person the disease has than what disease the person has.” – Hippocrates – Greek Physician (460 BC to 370 BC)
“It is far more important to know what person the disease has than what disease the person has.” – Hippocrates – Greek Physician (460 BC to 370 BC)
Hippocrates recommended willow tree bark extracts (similar to aspirin) for headaches, pains and fevers and also how to generate shared savings for Accountable Care Organizations. The top 5% of utilizers (“super-utilizers”) of health care services consume 50% of all spending or an average of $40,876 per year. To improve outcomes of super-utilizers, it may require taking the time to understand the person in addition to their clinical conditions. Their unmet social and basic needs may have contributed to their clinical condition and may prevent clinical treatments from being effective.
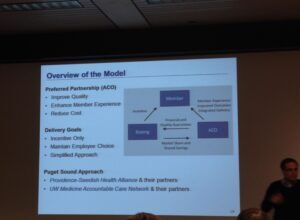
To develop this understanding, it requires more time than a typical office visit as well as listening and patience. It may require developing chemistry to build a connection and trust for patients to be comfortable sharing. These services are not likely to be reimbursable in the traditional Fee-For-Service model, yet they are essential for organizations in ACOs or Bundled Payments to generate shared savings. Once the patient’s unmet social and basic needs are addressed, their quality of life dramatically improves and the reduction of ER visits and hospital admissions may generate shared savings.
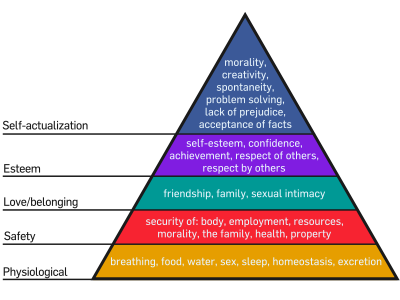
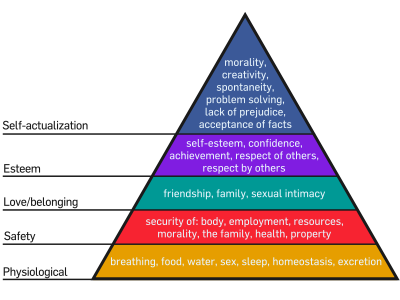
What are our social and basic needs?
Psychologist Abraham Maslow developed a “Hierarchy of Needs” theory that offers insight. The idea is that a person will not be able achieve the next levels of needs (i.e., manage diabetes or hypertension) unless the underlying layer is being met (food, water, sleep). It begins with our Basic Needs of Physiological (food, water, breathing, sleep) elevating to Safety (employment, resources, home). Our Social needs begin with Love/Belonging (friendship, intimacy, social interactions) then to Esteem (confidence, self-esteem) then the highest level which is Self-Actualization (creativity, sense of purpose).
How does addressing Social and Basic Needs generate Shared Savings?
The Pioneer ACO program started in January 2012. In the first year, CMS reported that $147M was saved across 23 organizations. The Montefiore Pioneer ACO generated $23M of that, resulting in being awarded $14M. This helps Montefiore fund their Care Management Organization that was established in 1996 to manage these reimbursement models as well as address high risk patient’s socials and basic needs.
Social
The quality and quantity of individuals’ social relationships has been linked not only to mental health but also to both morbidity and mortality. A study of 308,849 participants indicated a 50% increased likelihood of survival for participants with stronger social relationships. A study by the Journal of Clinical Oncology showed that married people with cancer were 20% less likely to die from their disease.
A study of Medicaid patients in New York hospital found that frequent Emergency Room users (10 or more ER visits per year) had many complicating factors in addition to their primary diagnosis. 77% had a chronic condition, 62% had history of substance abuse and 70% had a history of mental illness. Hospitals are not equipped to address their underlying social needs let alone address a multitude of clinical conditions. They are only paid to address the primary diagnosis. For the frequent ER users in the study, hospitals were paid to address their primary diagnosis’ which were chronic conditions 11%, substance abuse 12%, and mental illness 6% and other common reasons (i.e., flu or falls).
Montefiore found many of their patients with unmet social needs like being depressed or overwhelmed by being the primary care giver to someone else. Addressing these social needs may be required before clinical treatments are effective.
Basic Needs
A program in New York City has doctors prescribing fruits and vegetables to obese or overweight patients. The 1,000 Home Campaign is giving homes to the homeless, with their leader telling CBS’s 60 Minutes that “many of these people have such serious medical problems, it costs taxpayers more to leave them on the street.” University of Pennsylvania has doubled down on a program to hire and train Community Health workers to address patients basic needs.
Montefiore has found that the top 5 basic needs that need to be addressed are food, housing, finances, literacy, and transportation.
Our healthcare system is not designed to address social and basic needs. We don’t reimburse providers to do this unless the provider takes the risk, like Montefiore, to generate shared savings with the new reimbursement models. If the social and basic needs are not addressed, we will continue seeing patients like Dr. Jeffrey Brenner found that visited the hospital 141 in one year. Reducing the cost of healthcare and improving clinical outcomes may be more about addressing the social and basic needs of super-utilizers (50% of all spending) than clinical care.