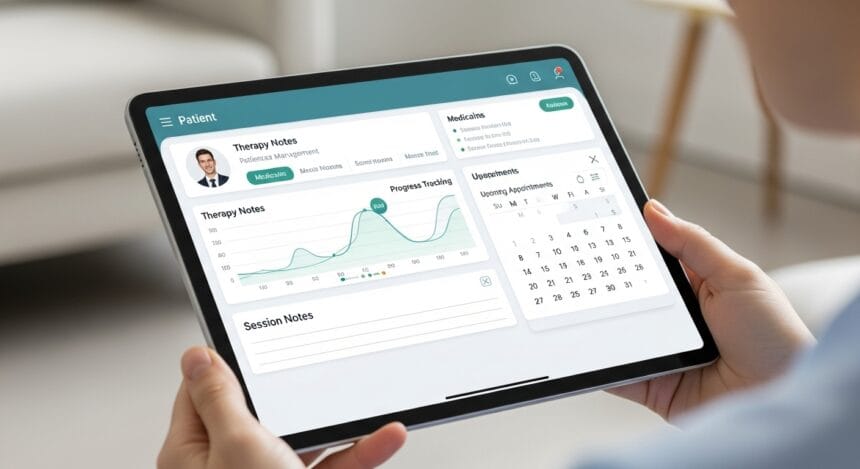
Electronic health records (EHRs) are now a core part of modern healthcare. In mental and behavioral health settings, they play a particularly important role in helping clinicians manage detailed notes, protect sensitive information, and follow a patient’s progress over time.
- Clinical Documentation and Progress Notes
- Secure Patient Records and Data Storage
- Scheduling and Appointment Management
- Treatment Planning and Ongoing Care Tracking
- Medication and Prescribing Support
- Billing and Administrative Workflows
- Patient Access and Engagement
- Reporting and Data Insights
- Interoperability and Information Sharing
- Turning Features Into Better Care and Smoother Workflows
But what should a mental health EHR actually do? While systems vary, most are built around core features that support clinical care, compliance, and day-to-day practice management.
This guide looks at those core features and explains why they matter for both providers and patients.
Clinical Documentation and Progress Notes
Clinical documentation sits at the core of any mental health EHR. Across healthcare more broadly, electronic records are now the norm. According to the Centers for Disease Control and Prevention, about 88% of office-based physicians use an electronic health record system, showing just how central digital documentation has become to everyday clinical practice.
In mental health care, this shift supports more consistent progress notes and a clearer, more complete picture of a patient’s history over time. Because therapy records are often narrative and session-based, EHRs are built to support formats such as SOAP, DAP, or BIRP, alongside structured fields for diagnoses and interventions. This makes it easier for clinicians to capture what happened in each session while keeping documentation organised and consistent.
Strong documentation tools also help clinicians review previous sessions, monitor changes in symptoms, and link care back to treatment goals. At the same time, they reduce the risk of missing or incomplete notes, which is essential for maintaining care quality and meeting compliance and reimbursement requirements.
Secure Patient Records and Data Storage
Mental health information is among the most sensitive data in healthcare. A core feature of any mental health EHR is the ability to store patient records securely while still allowing authorised access.
These systems are built with safeguards such as encryption, access controls, and audit logs that record who views or edits a file. This protects patient privacy and supports regulatory compliance, while ensuring clinicians can quickly find the information they need during care.
Centralized digital storage also means records are less likely to be lost or fragmented across different systems.
Scheduling and Appointment Management
Most mental health EHRs include tools for managing appointments and calendars, because sessions are the backbone of therapy-based care.
Scheduling features allow practices to book individual or group sessions, manage recurring appointments, and track attendance. When scheduling is linked directly to patient records, it reduces double-booking, reduces missed sessions, and keeps clinical and administrative information connected in one place.
This saves staff time and creates a smoother experience for clinicians and patients.
Treatment Planning and Ongoing Care Tracking
Mental health care is rarely a one-off interaction. It usually involves ongoing treatment plans that evolve as the patient progresses.
EHR systems support this by allowing clinicians to create and update treatment plans that connect diagnoses, goals, and interventions. Progress notes can then be linked back to these plans, helping show how day-to-day care supports longer-term objectives.
This makes it easier to review progress, adjust approaches when needed, and maintain continuity of care, especially when patients are seen over long periods or by multiple providers.
Medication and Prescribing Support
For practices that manage medications, many mental health EHRs include tools to record and monitor prescriptions.
These features help clinicians keep track of current and past medications, dosages, and changes over time. Some systems also highlight potential interactions or allergies based on the patient’s history.
Having medication information alongside therapy notes and diagnoses supports safer decision-making and provides a more complete clinical picture.
Billing and Administrative Workflows
Beyond clinical care, a mental health EHR often supports the practice’s business operations. This includes capturing billing codes, generating claims, and tracking payments.
By linking documentation directly to coding and billing workflows, EHR systems reduce the need for duplicate data entry and lower the risk of errors. This saves staff time and helps ensure clinical work is accurately reflected in reimbursement processes.
For many practices, this integration is crucial to maintaining efficient operations without adding extra administrative burden. In a recent survey, more than 60% of clinicians reported that documentation and administrative tasks significantly contribute to job stress and burnout, underscoring the importance of efficient, purpose-built record-keeping.
Patient Access and Engagement
Many systems now include patient portals or secure communication tools that allow clients to interact with their care outside of sessions.
With these features, patients can complete intake forms, send messages, and view portions of their records. This can reduce paperwork during appointments and help patients stay more engaged in their treatment between visits.
Better communication also supports stronger therapeutic relationships and clearer expectations on both sides.
Reporting and Data Insights
Digital records make it possible to analyze both clinical and operational data in ways that paper files cannot.
Reporting tools within a mental health EHR can help practices review outcomes, monitor caseloads, and prepare for audits or compliance checks. Over time, this data can also highlight trends, such as which approaches are working best or where workflows could be improved.
These insights support better decision-making at the clinical and practice level.
Interoperability and Information Sharing
As healthcare becomes more connected, EHR systems are increasingly expected to share data with other providers and systems when appropriate.
Interoperability enables the secure exchange of mental health records with primary care, hospitals, and health information networks using recognised standards. This helps ensure that mental health care is part of a broader picture of a patient’s health, rather than existing in isolation.
For patients with complex needs, this kind of connectivity can make care more coordinated and effective.
Turning Features Into Better Care and Smoother Workflows
A mental health EHR brings together documentation, secure records, scheduling, treatment planning, administrative workflows, and patient communication into a single digital system designed for behavioral healthcare.
At its core, it helps clinicians spend less time managing paperwork and more time focusing on patients, while supporting accuracy, privacy, and continuity of care.
Understanding these core features makes it easier for providers to evaluate systems and choose tools that truly support both their clinical work and the long-term health of their practice.