First published in MedCityNews.
First published in MedCityNews.
The dilemma of our age, in the words of bioethicist Dr. Ryan Nash, is asking what should be done in medical care, and not merely what can be done. “Often we’re facing innovations and technology that we can use a certain way, but a key question to ask is should we?”
 First published in MedCityNews.
First published in MedCityNews.
The dilemma of our age, in the words of bioethicist Dr. Ryan Nash, is asking what should be done in medical care, and not merely what can be done. “Often we’re facing innovations and technology that we can use a certain way, but a key question to ask is should we?”
Nash leads the Center for Bioethics at Ohio State University Wexner Medical Center and is the chair of medical ethics and professionalism. He also has a background in palliative care, having led the palliative care center at Cooper Green Mercy Hospital in Birmingham, Alabama.
In a recent interview, MedCity News asked Nash to share some of the challenges presented by recent advances in medicine and technology.
Let’s start with recent developments in medicine. What’s top of mind for a medical ethicist?
RN: Utilization of technologies, end-of-life planning, organ transplantation, all of those things are very much still important for ethics. We also have the realm of genetics and genomics, which in some ways the challenge is, what do we do with all of this information?
We now have the capability and the science to sequence genomes, but we don’t necessarily know which genes will be turned on or tuned off in a person, which can bring great dilemmas. So if someone carries a gene that indicates a higher risk of heart disease at an early age, I still don’t know if that gene will be expressed. Do I share that information with the patient? If I do, that means they might be more diligent in eating well, exercising, etc., but it also could add psycho-emotional pressure hanging over them like the sword of Damocles.
What about information technology. What dilemmas arise there?
RN: As we increase the flow of information from institution to corporation or institution to institution, we also have to ask what information should be shared? If genome sequencing becomes a regular standard, do I share that information with the insurance company? The concern there is, does something like the genome give a basis for inappropriate discrimination?
With EM Rs more is at stake than privacy issues, including questions around storing information in a way that is much more accessible and transferable than old paper charts. Many of the new systems are built for efficiency of linking billing to diagnostic codes and charting and not for what is the essential information the clinician needs to communicate with healthcare teams. So something as simple as an advance directive becomes a real challenge due to the process of getting those on an EMR and having that key information transported across care environments.
Rs more is at stake than privacy issues, including questions around storing information in a way that is much more accessible and transferable than old paper charts. Many of the new systems are built for efficiency of linking billing to diagnostic codes and charting and not for what is the essential information the clinician needs to communicate with healthcare teams. So something as simple as an advance directive becomes a real challenge due to the process of getting those on an EMR and having that key information transported across care environments.
Will these ethical dilemmas play out on a case-by-case basis, or will guidelines be developed?
RN: For something like organ transplantation, there have been groups that develop guidelines. With something like advanced care plans, states or large health institutions will form guidelines on how these things should be documented. But it’s far from a unified approach.
There are actually some dangers to systematizing. For example, advance care plans and living wills are generally thought of as good things. But the potential danger is that often patients and families are misinformed or uninformed. If advance care plans are done outside of the context of medical care, they may try to make too much of a distinction between, “we want to be allowed to die” or “we want aggressive life sustaining treatment.” In reality, many patients would more simply say, “I don’t want things that aren’t going to be helpful.” What is helpful is dynamic and situational and therefore difficult to systematize or put in an algorithm or guideline.
What are some of the innovations you would like to see, from a palliative care or ethics standpoint?
RN: With the original HIPAA, portability was the main goal. Since we don’t have a unified EMR in the U.S., portability is still a challenge. It’s increasing in some places, but I think we focus more on security and privacy than portability now. It’s important because it helps someone get the information they need quickly.
One of the innovations I would love to see is having an advanced care document that’s visible in the EMR. Right now, it may be buried somewhere in the EMR, but it’s not on the front page where it should be. If someone has terminal cancer and doesn’t want aggressive intervention or advanced life support technology, that should be clear to not just emergency room but paramedics and other clinicians.
Editor’s note: This interview was edited for brevity.
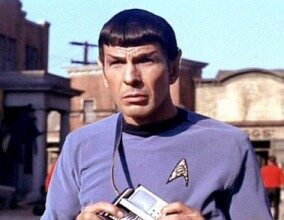
[Photo credit: Midwest Care Alliance]