Over one year ago my office implemented Allscripts Enterprise EHR (Electronic Health Record). I’ve not done a note on paper since. Last week, a “Transition of Care” (TOC) document was placed on my desk with a sticky note stating: “Dr. Nieder please fill out this form so we can bill a 99496 for your visit with Mrs. Jones yesterday”.
Over one year ago my office implemented Allscripts Enterprise EHR (Electronic Health Record). I’ve not done a note on paper since. Last week, a “Transition of Care” (TOC) document was placed on my desk with a sticky note stating: “Dr. Nieder please fill out this form so we can bill a 99496 for your visit with Mrs. Jones yesterday”. I pick up two sheets of paper with multiple questions including:

- Discharge Medications: (list)
- Present Medications: (list)
- Diagnostic tests reviewed/disposition (list)
- Disease/illness education (discussion documentation)
- Home health/community services discussion/referrals: (list)
- Establishment or re-establishment of referral orders for community resources: (list)
- Discussion with other health care providers: (list)
- Assessment and support of treatment regimen adherence: (discussion documentation)
- Appointments coordinated with: (list)
- Education for self-management, independent living and activities of daily living: (discussion documentation)
Please remember, I am now on an EHR. So I am expected to document in the EHR and THEN fill out these forms. I have no discharge summary yet from the hospital. It may be ready but no one bothered to send it to me and since our hospital is not sync’ed with our ambulatory clinics it sure didn’t seamlessly flow into my patient’s chart when she was discharged. When I finally do get it, there is no mention of any referrals given other than with the surgeon she saw in the hospital and me. The discharge medications state “resume pre-admission meds”. In order for me to list what tests she had and make sure they are normal I have to return to the hospital portal and look them all up. Some of them have already been scanned into the EHR. I have no idea if there were other referrals made but I doubt it. She had a very straight-forward admission for a small bowel obstruction. She declined to keep the surgeon’s appointment since they gave her instructions in her care in the hospital. I concurred about that. She could call them if she needed them. The women is a healthy 65-year-old who still works part-time as an accountant. She travels a lot.
This TOC visit is paid at a much higher rate than other visits IF the patient does not return to the hospital in the next 30 days. Hence, we hold the billing until that time.
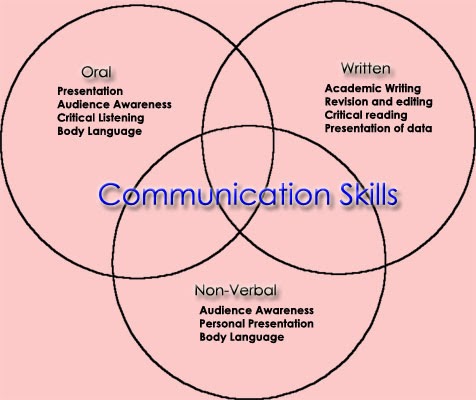
My understanding of the purpose of this new code is to improve the CO-ORDINATION of care as the patient transitions from the hospital to home. Coordination would imply that there are other individuals involved in giving the patient care and thus we should have improved COMMUNICATION
between us. However, at least in my institution, my staff and I bear the brunt of gathering information (which is what we normally do anyway, so I guess it’s nice because now we get paid for it).
At what point will it become incumbent upon the hospital, who I work for, to send me the necessary information for treating the patient now that he/she is home again? How does it follow that improving care means the primary care doctor fills out even MORE FORMS ultimately reducing the time spent with the patient? At what point does the operability of two disparate systems (office EHR and hospital EHR) talk to each other and the information I need is already in the EHR? Why isn’t all the information the patient needs sent home with her and she is told to bring that with her to her primary care doctor’s visit which, oh by the way, should be done within two weeks? Why aren’t all appointment made before she walks out the door?
The obvious answer is simple. What I am being asked to do is fill out a form so that my system can bill a 99496. The form will not keep the patient out of the hospital. Communication will keep the patient out of the hospital. True coordination of care might keep the patient out of the hospital. More busy work for the patient’s primary care doctor will not. Not in this universe or any other.
edited 10/9/2013 to improve specificity