Employers have seen their health care costs rise dramatically over the years. To compensate, they have expected employees to pay an increasing portion of the healthcare insurance premium, expected employees to pay significant co-pays with each physician visit and have purchased policies that restrict individuals to a narrow network of doctors and hospitals. Largely these have not worked. They have offset some of the expenditures but it has not done much to slow the inexorable rise of health care costs. The reason is because they attack the wrong “problem.” What is needed is to institute approaches to improve health and maintain wellness of the employee (and the employee’s family) and to assure that the employee (and family) get outstanding primary care including proactive population-style health care. Add to this patient engagement – a stake in the financial arrangement. That combination will reduce costs considerably. Here is one approach that progressive companies are following.
Large companies such as General Mills and Safeway have demonstrated the utility of wellness programs. Employees are invited to voluntarily participate in company sponsored programs that are designed for behavior modification such as nutrition, fitness, chronic stress reduction and smoking cessation. The employee (and sometimes the employee’s family members) who participate are rewarded with a reduction in their share of the health care premium. Given that employers are continually increasing employee share, this reduction can be a real benefit to a person’s paycheck. Large corporations often create these programs in house but smaller and many larger companies can turn to wellness companies such as Orriant that will do a turnkey approach for a single larger company or a group of smaller companies in a defined geographic region. Workplace wellness programs logically should improve employee health but until now results were mostly anecdotal; there was no definitive proof. Now, evidence has been published in the International Journal of Workplace Health Management that an opt-in program encompassing biometric testing and a personal wellness profile to guide individualized telephonic health coaching combined with financial incentives led to improved health parameters, improved health age and reduced healthcare costs. The authors concluded that “health coaching effectively improved biometric scores among high-risk individuals and narrowed the difference between current health age and achievable age, more so among those with the greatest health risks at baseline.”
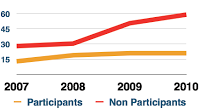
Here are some of the specific findings: Compared to nonparticipants, the participant’s claims paid increased at a lower rate and they had fewer claims per person. For those with elevated blood pressure, the average systolic pressure was 170 mmHg which was reduced by 34 over the three year study; for diastolic it was 105 down by 18 mmHg. For those with elevated glucose the starting average was 164.4 and dropped by 31(58%) over the three years. Those at the greatest risk for cancer improved their lifestyle score by nearly 32 points, or 41%.
According to those in the company wellness field, there are few key ingredients that make for a successful wellness program. The majority of employees (and spouses) need to be working one-on-one with a health coach to develop their own self-directed plan for behavioral improvement. Individual care and concern by the health coach is the most effective intervention. Employees need to like their coach (which I interpret to mean they trust their coach.) Coaches need to be well trained with a significant healthcare background. Individual accountability needs to be an integral part of the program. This implies that the participant needs to call the coach; not the other way around. That is part of accountability. The focus needs to be on those with health risks, which most Americans have. Getting the men in the company involved is important; women are more likely to volunteer early so there has to be extra effort to attract the men.
Some readers will not like the idea of health coaches “meddling in their affairs.” But no one is obliged to join into the wellness plan; it is always an option although for sure the employer often offers a financial incentive to do so. Whether in a wellness plan or affiliated with your PCPs office, health coaches (when properly trained and focused) have been found to be powerful advocates for improved health.
Major health risks from life style factors are being overweight (two thirds of the American population), lack of adequate exercise (probably more than half of people), chronic stress (it seems like everyone is stressed today) and smoking (still about 20%.). High blood pressure can be in part lifestyle directed as is obesity. These in turn lead to chronic illnesses such as heart disease, stroke, chronic lung and kidney disease – just the diseases that account 75-85% of all claims paid by healthcare insurance.
The cost of wellness programs, whether done in house or with a consultant, can be self-funding, i.e., those who opt in get lower premiums and those that do not have higher premiums. But the larger more valuable benefits accrue to both the employer and employee. Staff become healthier – that is good for them. But healthier employees use less total healthcare resources. This in turn lowers company insurance costs or at least slows the growth of premiums, often dramatically. The employee benefits from better health, will likely be more productive, will have less absenteeism and will have greater job satisfaction. That is a win-win for employee and employer alike.
My next few blogs will relate what some companies are doing to offer a complete package of wellness, prevention, consumer-directed insurance, on site primary care clinics, prefunding a HSA or HRA, price transparency and more to manage costs while improving employee health.
[Note: A look at the Orriant web site will show that I am quoted. I am a proponent of wellness programs but I have no financial or other association with the company. If you go to the link for the article on wellness plans noted above you will find that you need to pay to read more than the abstract. I read it and thought it was useful information which why I used it here. You can also find the details on the Orriant web site. As with any study there can be criticisms but I think it was pretty well done. The graph is claims paid per participant]