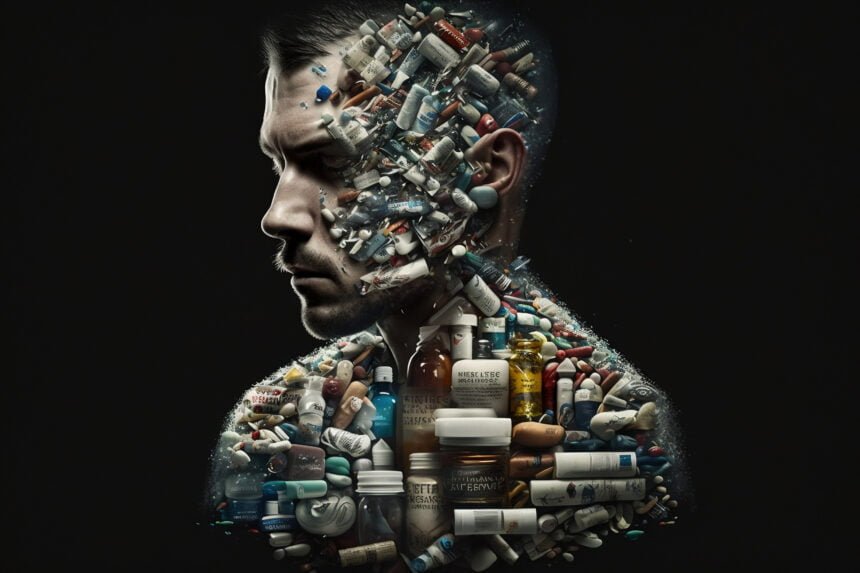
The recognition of co-occurring disorders, commonly referred to as dual diagnosis, marks a significant advancement in the understanding and treatment of complex mental health conditions. This term encompasses a range of combinations where a mental health disorder, such as depression, anxiety, bipolar disorder, or schizophrenia, coexists with a substance use disorder involving alcohol, drugs, or prescription medications. Historically, the healthcare system’s approach to these conditions often involved treating them as separate entities, leading to fragmented and less effective care. However, with the growing awareness of the interdependence between mental health and substance abuse, there has been a pivotal shift towards more integrated and comprehensive treatment models. These contemporary approaches aim to provide a more synchronized treatment plan, addressing the intricacies of each condition in relation to the other, thereby offering a more holistic path to recovery for individuals grappling with dual diagnoses.
This evolution in treatment strategies signifies a more empathetic and scientifically grounded response to dual diagnosis. By adopting integrated treatment models, healthcare providers can deliver care that is attuned to the unique challenges posed by co-occurring disorders. These innovative strategies often combine a variety of therapeutic interventions, including behavioral therapies, medication management, and support systems, tailored to meet the specific needs of each individual. The integration of these treatments acknowledges the complex and bidirectional relationship between mental health disorders and substance abuse, ensuring that both are treated concurrently rather than in isolation. This article delves into these cutting-edge approaches, exploring how they effectively address the multifaceted nature of co-occurring disorders and facilitate a more comprehensive and effective pathway to recovery.
Integrated Treatment Programs
Integrated treatment programs recognize mental illness and addiction cannot be viewed separately, as they fuel one another. Treating just one issue in isolation leaves the other still impairing the person. Integrated care uses a multidisciplinary team to simultaneously promote healing and functionality across conditions. Treatment components are coordinated, with the ultimate goal being sustained wellness. Patients are involved in setting personalized goals. Multiple recovery services are tailored to support patients in achieving their goals. Research confirms integrated treatment’s advantages for engagement, progress, and long-term prognosis compared to parallel or sequential treatment approaches.
Integrated care marks a paradigm shift to viewing the person holistically. Practitioners no longer bounce patients between mental health and addiction systems. They leverage the mutually reinforcing benefits of evidence-based interventions from both fields simultaneously. This unified approach empowers lasting change and skills patients can continue applying to manage their dual diagnosis beyond treatment.
Consumer-Driven Care
The traditional treatment model assigned patients passive roles, with practitioners as the sole authorities dictating interventions. Consumer-driven care instead recognizes patients as partners in their own recovery. It empowers patients to have a voice in shaping their care plans based on personal needs and values. Patients are involved in setting goals, designing programs, and evaluating progress. This fosters an empowering sense of control and choice, enhancing treatment buy-in.
Consumer-driven programs require flexibility to center services around each patient’s priorities. Patients can access information that helps them make informed decisions about treatment options. The customized approach makes recovery intrinsically motivating for patients. It also develops self-advocacy skills transferable to promoting their health beyond treatment. Consumer-driven care respects the fact that the patient is ultimately in charge of their recovery journey.
Holistic Wellness Services
Traditional treatment focused narrowly on managing psychiatric and addiction symptoms. Holistic services broaden the lens to nurture overall well-being. The mind-body connection is powerful, and activities like yoga and meditation can bolster mental health and recovery. Patients discover new tools for self-care and coping. Recreation therapy helps them rediscover passions and interests. Nutrition assists physical health. Expressive arts aid self-discovery and processing emotions.
Holistic modalities empower patients to be active participants in their own wellness. New coping skills build a life of purpose beyond disease management. Patients connect with core values to make choices aligned with what matters. Holistic care instills hope and self-efficacy. It ultimately equips patients with knowledge and tools to sustain their recovery and continue pursuing growth long after treatment.
Peer Support Groups
Shared lived experience provides a profound sense of connection and belonging. Peers intrinsically understand the day-to-day realities of managing co-occurring disorders. This empathy and validation is healing in itself. Knowing others relate reduces feelings of shame and isolation. Peers also offer invaluable practical guidance for navigating treatment, social services, and community resources. Informally sharing coping strategies provides hope and ideas.
Seeing peers successfully manage their disorders reinforces that recovery is possible. Peer supports empower patients to overcome obstacles. They modeled openness and honesty about the recovery process’s ups and downs. Support groups foster accountability, optimism, and skill building. The camaraderie makes a recovery feel less intimidating. Peers give patients a community to lean on throughout their journey.
Relapse Prevention Planning
Given the chronic nature of co-occurring disorders, relapse risks remain long-term. Prevention planning equips patients to minimize risks and handle warning signs appropriately. Patients gain insight into personal triggers and high-risk scenarios to avoid. Learning coping strategies and early intervention skills bolsters self-efficacy. Having a plan in place provides reassurance if old behaviors resurface.
Relapse prevention is not a solo endeavor. Planning includes identifying support people to reach out to. Troubleshooting potential obstacles promotes treatment engagement even during difficult times. Patients learn to reframe relapse non-judgmentally as an opportunity for more learning. Ongoing recovery is a process, not an endpoint. Effective planning treats relapse prevention as an evolving conversation that empowers sustainable change.
Medication-Assisted Treatment
Medications can be powerful tools for managing symptoms of mental illness and addiction. The right medication restores balance in brain chemistry to alleviate distressing symptoms. This enables patients to engage more fully in psychotherapy and behavioral interventions. However, medication alone is rarely a complete solution. Integrated programs thoughtfully incorporate medication alongside counseling, group support, and more.
Having on-site medical staff streamlines monitoring effectiveness and side effects. Medication is just one component of a comprehensive treatment plan tailored to the individual. The team helps patients develop skills for long-term wellness so medication becomes less necessary over time. Medical and psychosocial services work synergistically to promote functioning and quality of life. Medication assists the process but does not replace the hard work patients do to achieve sustainable recovery.
Trauma-Informed Care
Unaddressed trauma distorts a person’s worldview and sense of self. It understandably drives many maladaptive coping mechanisms like mental illness and addiction. Trauma-informed care compassionately acknowledges this link. All interactions aim to empower rather than inadvertently re-traumatize. Patients are viewed through a lens of resilience rather than damage.
Treatment establishes emotional and physical safety first. Patients regain power and control over their recovery. The team provides education on trauma’s impact and common coping strategies. Healing happens gradually as patients develop more adaptive skills for emotional regulation and relationships. Ongoing support groups help trauma survivors feel less alone. Trauma-informed care appreciates healing requires proceeding at the patient’s pace without judgment.
Assertive Community Treatment
Outpatient treatment has limits in assisting those with more severe co-occurring disorders. Such individuals often get caught in a revolving door of hospitalizations, incarceration, homelessness, and other crises. Assertive community treatment takes services out to clients in their natural settings. Addressing real-world needs makes treatment more practical and generalizable.
Multidisciplinary teams coordinate comprehensive care, including psychiatric services, addiction counseling, and case management. Services are tailored to each client’s changing needs. Proactive support increases stability, functioning, and quality of life. Teams help clients strengthen social connections and access community resources. Meeting patients where they are removes barriers to consistent treatment engagement. This intensive approach prevents crises requiring higher levels of care down the road.
Mindfulness Techniques
Living with co-occurring disorders often involves painful rumination and anxiety about the future. Mindfulness teaches present-moment focus to reduce distress. Meditation, yoga, and breathing re-center patients in the now. Observing thoughts and emotions without judgment builds equanimity. Mindful movement fosters bodily awareness. Simplified daily activities become opportunities to practice mindfulness.
Mindfulness provides tools to tolerate discomfort without impulsive reactions like substance use. Patients cultivate insight into their own thoughts, feelings, and urges. This self-awareness enhances control and emotional intelligence. Mindfulness also reduces perceived stress. With regular practice, it provides a portable coping skill for maintaining recovery in the long term. Patients learn to respond rather than react.
Dual Recovery Anonymous
Mainstream 12-step programs often alienate people with co-occurring disorders. DRA provides a tailored fellowship just for dual diagnosis. Members find shared understanding and holistic support. DRA honors that recovery is an ongoing process requiring a connection. The group adopted 12 steps to address both addiction and mental health.
DRA meetings allow open discussion of psychiatric symptoms and medication. Members serve as role models that show that recovery is attainable. The fellowship helps people reconstruct identities beyond being solely defined by their disorders. Ongoing participation provides community, accountability, and hope. Members draw strength from hearing others’ lived experiences. For many, DRA becomes a lifeline for maintaining dual recovery.
Conclusion
Treatment for co-occurring disorders has evolved considerably in recent years thanks to innovative approaches focused on integrated care. While managing dual diagnosis remains complex, holistic strategies that see the person beyond the symptoms offer much hope. Recovery is a journey, and emerging interventions help clients each step of the way. The future looks bright as new therapies continue to enhance the quality of life for those living with co-occurring mental illness and addiction.