(First published in the Harvard Business Review)

(First published in the Harvard Business Review)
In August, Dr. Donald M. Berwick presented the report from the independent National Advisory Group on the Safety of Patients in England (A Promise to Learn — A Commitment to Act: Improving the Safety of Patients in England) to Prime Minister David Cameron in London. The “Berwick Report” reflects on serious problems at the Mid Staffordshire NHS Foundation Trust that arose over several years, and the abysmal care received by patients at the trust’s Stafford Hospital in Stafford, England, during that time. I served on the advisory group, and I’m still asking how a trusted organization could deteriorate so completely without the leaders’ awareness or action? Could it happen elsewhere? How can we, as leaders, prevent these failures in the future?
As the report makes clear from the outset, there are lessons for all leaders in this story. I still see examples of what happened at Mid Staffs in even the best of hospitals. As we in the United States juggle major structural and operational changes and try to secure our financial systems as revenues fall, we must keep our promise of safety and high quality to every patient, every time. I offer three recommendations to ensure that we keep these promises to those who depend on our leadership.
1. Close the gap between the front office and the frontline
The leaders at Mid Staffs were focused on closing substantial financial gaps. This is a familiar and understandable concern and is usually the number one agenda item in many executive offices. But too often, I see leaders focusing on the monthly financials while losing connection to the work and care at the bedside.
Earlier in my career, I had the chance to visit leaders such as Jack Welch (GE), Paul O’Neill (Alcoa), and Ralph Larsen (Johnson & Johnson). Each described a core part of their weekly work as “walks of shame.” They described their regular visits to see the work going on at the frontlines and being both ashamed and humbled when they saw the impediments to quality and the risks to safety. They’d return to their offices inspired to improve processes and remove barriers for the people doing the frontline work. They were committed to listening to the concerns that staff shared, seeing the complicated workarounds that broken processes necessitated, and leading change in order to make quality the priority. They created and maintained a close connection to frontline staff — what Jim Womack, the expert in lean production and thinking, calls “going to gemba” — Japanese for “the actual place.”
At Mid Staffs, instead of this essential connection, there was a yawning gap. When frontline workers raised concerns about staffing levels, experience on the night shifts, and supply shortages, the Mid Staffs leaders walked away from leading. They stayed away from the wards, rebuffing the expert knowledge that could have protected dignity and saved lives. The staff came to work each day filled with anger and desperation and, in many cases, took out their frustration on the helpless patients in their care.
Leaders need to build reliable processes to hear the staff. Some of the best leaders I know have created effective ways to ensure daily interaction among all leaders, caregivers, and patients. Rob Colones, CEO at McLeod Health in Florence, South Carolina, has every senior leader start his or her day by rounding on units and talking with staff and patients. John O’Brien, former CEO at Cambridge Health Alliance and the University of Massachusetts Health System, held monthly breakfast meetings with any staff who had been patients in the system that month or who had family in the hospital. At the breakfasts he asked, “What rules did you break to make your care great?” His agenda became lowering or removing those barriers staff were working around.
2. Ask four questions
On my visits to health care organizations, I often ask these four questions to assess the overall level of quality and to understand how the leaders drive for best performance:
- Do you know how good you are?
(I’ll look at the dashboards or other quality reports they use to measure performance. I’ll also ask about the qualitative methods the leaders use to understand the patients’ views on their care.)
- Do you know where you stand relative to the best?
(Most often, leaders look at their own performance. But when they know how big the gap between them and the best performers is, they are inspired to change.)
- Do you know where the variation exists?
(Most leaders still look at averages and miss the opportunity to build will for improvement by assessing the entire range of performance across various providers and departments.)
- Do you know the rate of improvement over time?
(Many leaders overestimate their progress. The data on rates of change over time compel new improvement progress.)
These questions help focus attention on the right things and set the right priorities. They communicate the necessity of understanding quality as a living, changing thing, not as a static metric. And they also impart a healthy dose of competition — the kind that leverages curiosity and pride to generate learning.
3. Build reliable and effective ways to hear the voices of the patients and family members
The Mid Staffs leaders used only basic methods to hear the voice of their patients and family members. The most effective leaders have reliable and vibrant ways to seek out input from patients and families on designs of services, programs, and care models. Effective leadership creates easy ways for patients to offer complaints and reliable processes to respond to patients and resolve the issues. This requires much more from leaders than reviewing survey results. Leaders in the best systems have ways to hear the good and bad outcomes of care, and they have effective systems for improvement.
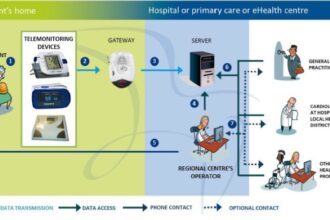
At Ryhov Hospital in Jönköping, Sweden, patients now administer their own dialysis treatments, in much the same way as we now bank for ourselves at ATMs and fill our own gas tanks. This innovation developed because the frontline staff had strong, trusting, and supportive relationships with the patients they cared for and had strong improvement skills. The mid-level leaders could assess the real effects of personalized care and measure the impact against all aspects of the Institute for Healthcare Improvement’s Triple Aim: simultaneously improving the health of their population, improving the quality of care they received, and reducing costs per capita. And the senior leaders, having built a culture of patient-centeredness and improvement, could see the potential for new care models in hearing the voice of the patients.
The failures of leadership at Mid Staffs had to do with attention. Their attention was on their finances — understandable and even appropriate these days. But attention isn’t limitless, and faced with financial and business model pressures unlike any we’ve seen, it’s easy to spend too much of it on the wrong things. All of us need to pay attention, in person, to the work at the frontlines. We need to pay attention to our systems for building effective teams to execute on work and improve. And we need to pay attention to creating and maintaining reliable ways to seek, hear, and integrate the voices of our teams, and the voices of our patients.