Healthworks Collective tries to explore connections in medicine that are often overlooked in everyday care. It is especially focused on how different body systems influence one another in ways that affect long-term wellness. You can see this approach clearly when examining the link between foot health and vascular function from a clinical perspective.
You may not immediately associate foot discomfort with circulation concerns. It is a connection that becomes clearer when symptoms are examined together, and clinicians are paying closer attention to this relationship. Keep reading to learn more.
Understanding the Clinical Link Between Feet and Blood Flow
You can observe that the feet are often the first area where circulation problems become visible. There are signs such as temperature changes, skin color shifts, and delayed healing that point to vascular involvement. A report by the American Podiatric Medical Association states that almost 8 in 10 Americans have experienced a foot problem. It is a statistic that highlights how common foot-related issues are across the population.
Foot health isn’t just about proper footwear and nail care, it’s intricately tied to vascular function. When it comes to preventing limb loss and managing chronic conditions like diabetes or venous insufficiency, the collaboration between podiatrists and vascular surgeons is not merely helpful, it’s essential. This clinical intersection is critical to improving patient outcomes, particularly among populations at risk for peripheral artery disease (PAD), non-healing ulcers, and lower limb amputation. Proximity and partnership between these two specialties can be a game-changer, especially in high-risk regions like Miami. Learn how combining vascular and podiatric expertise leads to comprehensive care within a multidisciplinary hospital environment like South Florida Multispecialty Medical Group.
It is common for patients to dismiss foot pain as a normal part of aging or daily activity. You may not realize that these symptoms sometimes reflect deeper circulation concerns rather than surface-level strain.
You can also see how vascular conditions influence foot health over time. There are reduced blood flow patterns that limit oxygen delivery to tissues and slow recovery. Todd Neff of UC Health reports that one in four American adults have a vein issue. It is a figure that helps explain why foot symptoms often overlap with vascular disorders.
It is often during routine exams that clinicians notice early warning signs in the feet. You can benefit from these observations when they lead to earlier evaluation of circulation health.
You may notice swelling, numbness, or aching that worsens after long periods of standing. There are cases where these symptoms reflect venous pressure changes rather than joint or muscle problems.
It is helpful for clinicians to assess foot structure and skin condition alongside pulse strength. You can gain a clearer picture of vascular health when these factors are reviewed together. There are practical screening steps that improve detection of circulation-related risks.
You can improve outcomes when foot care and vascular assessment are treated as connected rather than separate concerns. It is a clinical mindset that supports earlier intervention and better long-term monitoring.
You may reduce complications when foot symptoms prompt timely vascular evaluation. It is through this combined focus that clinicians can better protect mobility and overall health.
The Biomechanics-Circulation Connection
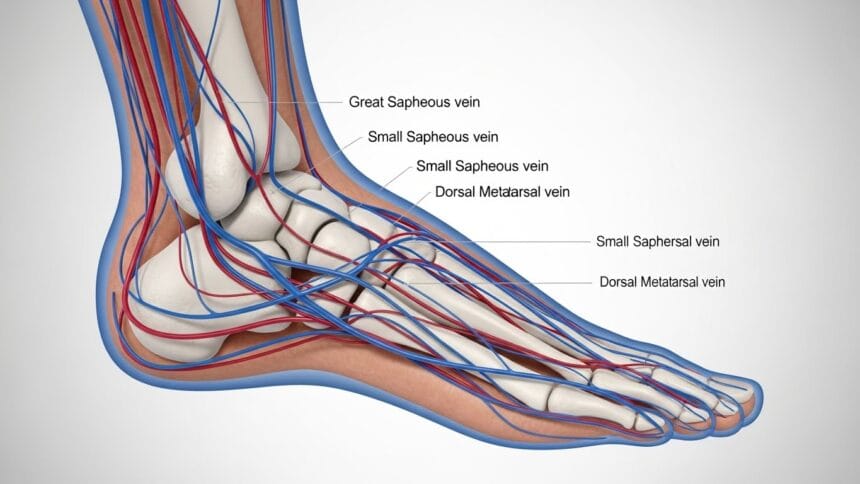
A complex relationship exists between lower extremity biomechanics and vascular performance. Abnormal loading, limited joint mobility, or improper gait can compromise blood flow through the foot’s arterial and venous systems. Conditions such as flatfoot, bunions, and plantar fasciitis may seem orthopedic in nature, but they can impact vascular health by altering the mechanics of blood return and supply.
Podiatrists assess gait patterns, foot structure, and pressure distribution, all of which may signal compromised circulation. Meanwhile, vascular surgeons investigate arterial blockages or venous reflux that could worsen these mechanical issues. A synchronized evaluation offers a full-picture approach to managing foot pain and circulation problems, streamlining treatment strategies.
Vascular Disease and Foot Complications
Peripheral artery disease affects over 6.5 million people in the United States, many of whom will experience leg pain, cramping, or foot ulcers due to poor blood flow. Without early detection, minor foot wounds can develop into gangrene or require amputation. That’s why podiatrists and vascular surgeons must work together in both preventative and reactive care pathways.
In regions like Miami, where diabetes prevalence is significant, podiatry services in Miami are often the first line of defense. Through regular foot care, high-risk patients are monitored for skin integrity, tissue perfusion, and pressure ulcers, then referred seamlessly for vascular scans and treatment if ischemic signs are present.
Venous Insufficiency and Lower Extremity Health
While much attention is given to arterial disease, venous disorders also play a vital role in foot and ankle health. Venous insufficiency characterized by incompetent valves and poor venous return often leads to leg swelling, skin discoloration, varicosities, and venous ulcers. These symptoms manifest primarily around the lower legs and feet.
Vascular surgeons typically manage venous ablation, sclerotherapy, or compression protocols. However, podiatrists contribute by managing ulcer offloading, preventing infection, and correcting orthopedic imbalance that contributes to stagnant flow. This dual-role care model reduces recurrence and accelerates healing in complex venous cases.
The Role of Medical Aesthetics in Surgical Recovery
With the rise of medical aesthetics in postoperative recovery, options like laser therapy, lymphatic drainage, and hormone support can aid tissue regeneration and cosmetic outcomes. After foot surgery or vascular interventions, these therapies help manage swelling, bruising, and scar formation.
For example, patients undergoing hormone replacement therapy in Miami have reported faster healing and improved vascular elasticity, supporting both surgical and aesthetic outcomes. Integrating these non-invasive modalities into the care continuum aligns with patient-centric recovery goals.
The Multidisciplinary Model
A multidisciplinary hospital in Miami offers one of the most effective frameworks for uniting podiatrists, vascular surgeons, endocrinologists, and wound care specialists. This coordinated approach reduces time to diagnosis, facilitates real-time communication, and ensures patients receive wraparound care. Within one facility, providers can collaborate through shared health records and collaborative case reviews.
Such models are essential not only for treating complex cases but also for early intervention. For instance, routine vascular screenings embedded in podiatric evaluations help catch worsening conditions before they progress to limb-threatening stages.
Clinical Decision-Making Framework
When to Refer: Podiatrist to Vascular Surgeon
Podiatrists should refer patients for vascular consultation when they observe signs such as diminished pulses, cool extremities, non-healing wounds, or discoloration. These indicators suggest underlying arterial insufficiency requiring imaging and possible intervention.
When to Refer: Vascular Surgeon to Podiatrist
Conversely, vascular surgeons managing ischemic limbs should involve podiatrists for gait evaluation, wound debridement, orthotic management, and post-procedure foot monitoring. This ensures long-term mobility and lower extremity function is preserved.
There’s no denying that podiatrists and vascular surgeons are stronger together. From preserving limb integrity to improving quality of life, interdisciplinary care is crucial. As our healthcare system continues to evolve, specialties must collaborate, not operate in isolation. If you’re looking for integrated care from podiatry to vascular health, consider learning more about comprehensive podiatry services in Miami at South Florida Multispecialty Medical Group.