Frequent Emergency Room users (10 or more ER visits per year) averaged 10 physician office visits per year, according to a study published in Health Affairs. It offers insight into frequent Medicaid ED users in New York City.
Frequent Emergency Room users (10 or more ER visits per year) averaged 10 physician office visits per year, according to a study published in Health Affairs. It offers insight into frequent Medicaid ED users in New York City.
 Frequent Emergency Room users (10 or more ER visits per year) averaged 10 physician office visits per year, according to a study published in Health Affairs. It offers insight into frequent Medicaid ED users in New York City. The study also demonstrated that our healthcare system is built around “patient services” rather than “patient recovery.”
Frequent Emergency Room users (10 or more ER visits per year) averaged 10 physician office visits per year, according to a study published in Health Affairs. It offers insight into frequent Medicaid ED users in New York City. The study also demonstrated that our healthcare system is built around “patient services” rather than “patient recovery.”
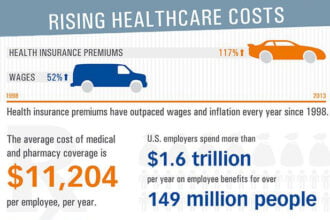
A key premise of the Affordable Care Act (Obamacare) was that by expanding Medicaid coverage, it would reduce expensive ER usage because patients would get care from primary care physicians. Yet New York Medicaid patients with 10 or more ER visits per year averaged 7 primary care visits, 2.5 specialty care visits and 1 OB/GYN visits during the same year.
If all we do is cover more people with Medicaid, we may get more ER visits than less according to a study from Science. It found that in Oregon, people of the same demographic that enrolled in Medicaid had 40% more ER visits than people that remained uninsured.
The reasons patients are in the ER are complex and many. The patient may be very sick or their physician office may be closed (nights, weekends) or not accessible (transportation). Their primary care physicians may have found their case to be too complex for the 7-10 minutes they can afford to spend with patients based on the Medicaid reimbursement.
The ER may be all that fits into a patient’s complex life as described by this patient: “When I go to my primary, I don’t have a copay. I don’t have a copay in the ER either. But my primary care doctor may send me to 2 or 3 specialists, and sometimes there is a copay for them. Plus time off from work to go see them. It’s cheaper to just go to the ER.”
If enrolling people in Medicaid will not fix the overuse of expensive ER services, what will?
The answer may come from Oregon Medicaid’s new Care Coordination Organizations (CCOs). These CCOs take a holistic view of Medicaid patients by addressing the many contributing factors to the ER visit. In the first 9 months of the program, the CCOs decreased ER visits by 13% and reduced hospital admission for heart failure by 32%, COPD by 36% and Adult Asthma by 18%.
It may take addressing each of the 14 categories of patient recovery factors to reduce excessive ER use like the Oregon CCOs have begun to demonstrate:
- Patient (About) – Do they have family close by? Will the family help? Are they dealing with a recent stressful event or coping with stress?
- Clinical Condition – What are their contributing chronic conditions (Diabetes, COPD, Heart Failure)? What are their behavioral health issues (i.e., substance abuse, depression)? Do they have any impairments (i.e., visually impaired, loss of limb)?
- Functional Conditions – Are they able to take care of their personal needs (i.e., bath, cook food)? Are they able to walk or go to work to earn a living?
- Patient Activation – Do they understand their clinical conditions and how to treat them? Can the diabetic patient effectively monitor glucose levels and properly inject insulin? Are they taking their medicine, eating nutritional foods and keeping their physician appointments?
- Socioeconomic Status – In the United States, 38% of people with chronic conditions and 58% of the uninsured did not see a doctor when sick because of cost.
- Physical Setting and Environment (Home) – Is their home or facility (nursing home) appropriate for their situation including heat, air conditioning, wheel chair accessibility, supportive other residents? Is the housing temporary (Shelter, living with family member)?
- Patient Preferences – What are the patient preferences (living will, technology use, treatment, palliative care)?
- Patient IT adoption – Only 6% of the people in the United States exchanged emails with physician in past 2 years. Are they willing to use text messaging or remote activity monitors? Do they have an online Medical Record? Are they able to access the patient portal?
- Access & Logistics – Are they able to take time away from work to see a doctor? Do they have the transportation? Are they getting nutritional food delivered to their home? Do they need medical transport?
- Recovery Team – Who are their clinical providers and are they sharing information? Do they have care givers (Family members)? Are there community support services (i.e., Meals on Wheels, Smoking Cessation Programs)?
- Recovery Goals – What are the recovery goals? Clinical conditions (blood pressure levels)? Functional conditions (back to work, see grandchildren soccer games)? Patient activation (able to treat conditions)? Physical setting and environment (live independently at home)?
- Recovery Plan – What are the prescribed medicines, therapies, procedures and surgeries? How will each of the patient recovery contributing factors be addressed? What are their qualified recovery options (cost, time away from work, surgery success rates, side effects, etc.)?
- Recovery Monitoring – What will be monitored (weight, blood pressure, medication adherence)? By who? How?
- Recovery Management – What do you do if the physiologic metrics are outside the defined threshold? When do you call if conditions worsen or you think you’re having adverse reactions to a new medicine? Who do you call?
Emergency room patient / shutterstock