Certainly one of the methods to reduce fraud is to catch the opportunists that see the U.S. Treasury as easy pickings. Hidden in the maze of billing, coding, electronic claims is software coding that can easily be turned to the white collar thieves.
As physicians we need to be aware of the potential of careless, negligence and even possible misuse of your own billing system. The buck stops and starts in your very own office.
Fraud can be construed when a charge is made for a procedure that has not been performed, or with creative ‘up coding’ to a higher management code. Another common procedure is a ‘storefront’ phantom medical practice.
LOST MONEY
Medicare billing errors, excessive payments and fraud have cost U.S. taxpayers hundreds of billions of dollars over the past decade. Medicare’s annual estimates, however, do not account for all fraud nationwide.

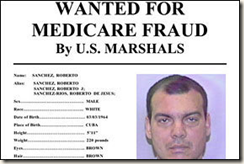
FRAUD PROSECUTIONS
Federal prosecutors in South Florida scratched the surface of Medicare fraud in the 1990s. But it wasn’t until a few years ago that they began to crack down on the corruption. Today the region’s prosecutions account for more than one-third of all Medicare fraud cases nationwide.

Read more here: Miami Herald
Medicare fraud rampant in South Florida
BY JAY WEAVER
jweaver@MiamiHerald.com
Whenever Alexander McCray lights up his crack pipe, U.S. taxpayers help pay for his habit.
McCray has defrauded Medicare by selling his government-issued health card number to private clinics in exchange for kickbacks of $150 to $300 a visit — as often as three times a day, three times a week over seven years, according to federal records and his own admission.
McCray has signed off on phony infusion treatments for his HIV illness — therapy that is medically obsolete — and he has received thousands of dollars from Medicare-licensed clinics all over South Florida.
Money that he has used to buy crack cocaine.
Dozens of clinic operators have in turn filed more than $1.1 million in false claims for fabricated HIV-infusion treatments billed in his name, according to Medicare records reviewed by The Miami Herald. Some 90 doctors, including one indicted in May, appeared on the phony prescriptions written on behalf of McCray.
”I’m the king of it all,” the 40-year-old, unemployed Opa-locka man told The Miami Herald recently, when asked about his Medicare scams.
McCray, a ”professional patient” with a 15-year criminal history of drug possession, is among thousands of con artists who have made South Florida the nation’s capital of Medicare fraud. A six-month Miami Herald investigation has found that the corruption has spun out of control during the past decade with little effort by Medicare regulators to stop it here and in other major cities. This past week, during a policy forum to confront the crisis, federal lawmakers said Medicare fraud costs taxpayers nationwide at least $60 billion a year.
Read more here: Rampant Fraud in South Florida
And in Brooklyn, New York
Federal agents raided health care facilities in nine states this morning, arresting dozens of suspects believed to be defrauding Medicare of tens of millions of dollars.
Federal authorities say this is one of the largest — if not the largest — take-down of Medicare fraud suspects ever conducted.
The raids began in morning in the pre-dawn hours. The targets: more than 100 doctors, nurses, therapists and healthcare company executives who have allegedly been stealing tax dollars to the tune of $200 million in recent months. Much of the fraud involved healthcare professionals billing the government for medical services never performed and medicine not provided.
Investigators say the Brooklyn scheme worked like this: Patients willing to go along with the scam were paid $40 per visit for three appointments per week, and were often diagnosed with vertigo or other ailments that would limit their mobility. Ambulettes provided by Medicare and Medicaid were transporting these patients back and forth for fraudulent appointments.
The clinic would then collect from Medicare or Medicaid for the ambulette rides, and the supposed services provided at the phony appointments. Taxpayers were billed millions for unnecessary treatment or treatment never provided.
The raids were conducted in Miami, Brooklyn, Tampa, Chicago, Baton Rouge, Houston, Dallas, and Los Angeles.
The Whistle Blower, and How to Report Fraud
Here is another ‘tale of deceit’
A combination of events created this break in security.
Medicare received a series of paper claims for diabetic retinopathy laser photocoagulation from an ophthalmologist’s office. They were unusual, claiming a series of 8 treatments in a series for proliferative diabetic retinopathy. While a series of PRP for PDR is not unusual 8 is highly unusual. This medical practice used electronic billing exclusively, yet the claims were on paper forms. Each paper claim totaled 25,000 dollars and there was a series of claims totaling $ 875,000. The patient identification numbers and locations were not from the usual practice locations.
The paper claim had the correct MD name, Medicare Provider ID practice location ICD and CPT coding.
These events tripped off the Medicare fraud alert system. At the time the practice had been sold to another MD and a transition was in place. The original physician had relocated the to another state.
The claims were for procedures performed after the original physician had closed his medical practice.
The attorney general contacted the physician with many open-ended questions possibly suspecting the physician himself was the perpetrator of the fraud. It became readily apparent that this was not the case.
This physician’s Medicare provider ID was compromised by a lack of security. It’s important to remember that your insurance ID numbers are much like a credit card number, and are perhaps less secure since they do not require PIN numbers. The information is handled by many personnel in the billing office. In this particular situation there was also a change in office personnel.
It was determined that a previous biller was part of a scheme to defraud Medicare, either selling or giving the Medicare numbers to acquaintances who knew enough to use them to defraud the taxpayer of almost a million dollars.
A ‘sting’ operation went into operation allowing the thieves access to the money cashing their checks and tracing the money to a racetrack and a person attempting to cash the US Treasury check. Even more interesting was the checks were negotiated at a well known horse racing track in the greater LA metro area.
The perpetrators were confronted at the teller window by several FBI agents who inquired how they got the checks. The suspect turned around and said, “from that doctor over there’… (there was no “doctor over there”.
Fast forward about a month, when the MD received a call from an FBI agent who asked him to send him a copy of a photo of himself, a driver’s license and a sample of his signature and writing sample. Even though completely innocent the physician realized how easily he could have been implicated.
As events turned out he was found to be an innocent victim of the scheme. He was required to appear before a grand jury where the guilty perpetrators were indicted, tried and sent to prison for felony fraud.
This was my personal story…it happened to me
This scenario while somewhat unusual is not unique. The moral of the story…treat your ID numbers as if they were credit cards, and if you make paper claims do not allow them to be known other than by your billing personnel.