Just like other people, doctors come in all sizes, including L and XL. How, you may be wondering, does physician size (as measured by BMI) impact care of overweight/obese patients?
Just like other people, doctors come in all sizes, including L and XL. How, you may be wondering, does physician size (as measured by BMI) impact care of overweight/obese patients? This was the question researchers (Sara Bleich et al) at Johns Hopkins Bloomberg School of Public Health attempted to answer in their study, “Impact of Physician BMI on Obesity Care and Beliefs” published in the May 2012 issue to the journal, Obesity.
Five hundred PCPs (General Practitioners, Family Practitioners, and General Internists) were randomly chosen from the Epocrates Honor panel, an opt-in panel of 145,000 verified physicians in the US. The sample was drawn to match physicians in general for age, gender, and region of the country.
The physicians were asked to self-report their BMI. Based on that, they were categorized as normal (47%), overweight (38%) or obese (15%). Two underweight physicians were removed from the sample leaving 498 participants in the study. Because there were so few obese physicians, overweight and obese doctors were lumped into one group for purpose of analyzing outcomes.
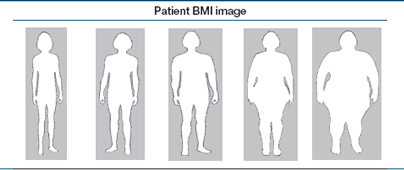
Via a survey, the docs were asked to provide additional information, including whether they had received good or very good obesity-related training in medical school or residency. They were also shown drawings of people with five different categories of weight (normal, overweight, Classes I-III obesity) and were asked to choose at which size they would typically initiate a weight loss discussion and record an obesity diagnosis. Finally, the subjects were queried on a variety of attitudinal topics, such as “whether patients trust weight loss differently if provided by an overweight/obese physician.”
Here is what they found:
• Physician BMI did not impact whether a doctor recorded a diagnosis of obesity. It did, however, impact whether or not the physician engaged the patient in a weight loss discussion. Overweight/obese doctors were significantly less likely than their normal weight counterparts to discuss weight loss with their Class II obese patients (BMI, 35.0-39.9) – 18% vs 30%, P= 0.010. The relationship persisted even after the researchers adjusted for other factors, including weight loss intention, obesity training, region of the country.
• Overweighs/obese physicians played down the importance of being a role model with 56% (vs. 72%, P=0.002) strongly agreeing that “physicians should be role models by maintaining healthy weight” and 57% (vs. 73% P=0.001) strongly agreeing that physicians should be role models by exercising regularly.
• Compared to normal weight doctors, obese/overweight physicians had significantly lower self-efficacy for providing lifestyle counseling, although they tended to report higher self-efficacy for prescribing weight loss medications compared to normal weight counterparts.
• Interestingly, overweight/obese doctors more often strongly agreed with the statement “I am usually successful in helping my obese patients lose weight” – although the numbers were small in both groups (5% vs 2%, P=0.034).
• Normal weight docs were more likely to believe that overweight/obese patients would be less likely to trust weight loss advice from overweight/obese doctors (79% vs. 69%), P=0.03).
• Finally, and this is fascinating, overweight/obese doctors more frequently documented an obesity diagnosis (93% vs 7%) and discussed weight loss (89% vs. 11%) when the physician’s perception of the patients’ body weight met or exceeded their own personal body weight.
Although many physicians express frustration when trying to get their patients to lose weight, it is important that they help their patients recognize obesity as a health problem and that they discuss weight loss options. As is the case in other “lifestyle problems,” such as excessive drinking, cigarette smoking or domestic violence, physicians’ acknowledgement and support are documented to be helpful, even if patients cannot (or will not) initially comply with the recommendation.
On the other hand, failure to diagnose and counsel patients on these issues can have the opposite effect, sending a message that the doctor does not see the issue as a problem worth discussing. I can only imagine that an overweight/obese physician that fails to diagnose and counsel on obesity could send, pardon the pun, an even bigger message: “Look at me, I am not worried about my weight, so why should you worry about yours?”
The authors are careful to say that targeting overweight/obese physicians for special training was probably not the right answer. After all, most physicians, obese or not, were not diagnosing or counseling patients in the overweight category (BMI 25.0-29.9) when arguably getting to a normal weight would be easier than once someone is much heavier. They do suggest, and I agree, that a better (although untested) tactic might be to focus on physician well-being by encouraging healthy lifestyles, including diet and exercise.
One thing not raised specifically in the article is what kind of care these doctors are getting from their own doctors. How many overweight/obese doctors are being actively encouraged by their PCPs to eat better, exercise more, and lose weight? For that matter, how many of these doctors even have doctors? And, if they do, do they actually function as the patient in the doctor-doctor dyad?
Since doctors are not immune to the health impacts of obesity, perhaps the doctor’s relationship as patient could be a good place to start.
Perhaps this would be a place to start.