Mobile asset management in the hospital is a great example of an unsexy but high-impact topic. In this interview, John McCarthy, GE Healthcare’s GM of Asset Management Professional Services, answers my questions.
1. What financial challenges are on the minds of C-level executives at US hospitals?
Mobile asset management in the hospital is a great example of an unsexy but high-impact topic. In this interview, John McCarthy, GE Healthcare’s GM of Asset Management Professional Services, answers my questions.
1. What financial challenges are on the minds of C-level executives at US hospitals?
Clearly, there is uncertainty surrounding the future of health care reform. We hear from our clients that reimbursement implications, quality improvement and expense reductions are their top challenges. This is also supported by the most recent ACHE CEO survey that was released in February 2012. Put plainly, hospitals must provide higher quality patient care with fewer resources at a lower cost. It’s crucial that while cutting cost, the quality of care must improve.
2. What is driving the rise in “clinical assets” across hospitals, and how does this impact a hospital’s bottom line?
As technology has become progressively more advanced and more tightly integrated into patient care, the number of devices has exploded. Consider that in 1995, there were eight devices at the bedside – in 2010, there were 13. There are many reasons for this growth, including more treatment options and introduction of advanced technologies, among others. With the additional requirements in reporting and maintaining quality care, caregivers no longer have the time to look for equipment and require technology to be readily available. If equipment is not readily available, they will request to buy more and while purchasing the equipment is an obvious financial expenditure, the commitment to an asset expands to service, maintenance and user training, among other elements – all of which can have a financial impact. At 95 percent of an organization’s “clinical asset” base, mobile assets can number in the thousands and represent tens of millions in total investment.
3. Why are assets so difficult to track within hospitals?
There are a number of factors. Most simply, many assets are mobile and can end up in the “wrong” place. Also, if existing processes don’t put equipment in caregivers’ hands when they need it, they will often circumvent ineffective processes to meet their specific needs or “just in case” of an unplanned need. This can mean they hoard equipment.
More importantly, few hospitals have clearly delineated responsibilities for all the steps required for managing assets not actively engaged in clinical care (such as removal from the area of care, cleaning, redistribution to stocking locations, tagging inoperative equipment). Today, most hospitals manage mobile assets in a random, transactional way. In many instances, there is no reliable, systematic process to ensure that, for example, a nurse can locate a clean, usable IV pump when a patient needs one. When everyone in general has responsibility, no one person has any accountability.
But the larger problem at hand is largely utilization – or the amount that assets are actually used in patient care. On average, utilization for mobile devices is only around 42 percent, meaning that equipment is not being used to full capacity and resulting in a bloated and underused asset inventory.
4. How does ineffective management of assets impact productivity in today’s hospital?
Most health care organizations do not make the connection between acquiring devices and usage patterns or clinical needs. We find that, in general, hospitals have around 25 percent more mobile devices than can even be used. So, the first impact on productivity comes from the equipment itself through decreased utilization.
It’s common to find assets that haven’t been used in over 30 days. This means that the equipment is pooling in areas of low demand rather than being located at the right place and in the right condition for clinicians who need them. In turn, these clinicians search for the equipment or make multiple calls in the hope that someone else will do it for them. This search time is the second impact on productivity.
5. What actions can health executives take to start better managing assets?
While the process of auditing how many clinical assets are in a facility and understanding how, where and when they are used is certainly a large undertaking, there are a few steps crucial to getting things under control. First, conduct a physical inventory to get a better view into what the facility already has. At GE Healthcare, we’ve found that most hospitals we work with are initially off by at least 60% in inventorying mobile clinical assets.
It’s important to note that cutting down inventory alone won’t fix under-utilization – workflow plays a huge role. So, executives also need to optimize workflow before adjusting the number of assets. And finally, executives should develop a replacement strategy for equipment. Often, the purchase of equipment is driven by subjective observations such as “we have trouble finding telemetry monitors in this nursing unit.” The real question to ask is: why are they hard to find? Feedback and requests should be balanced against a strategic plan for equipment replacement.
6. What sort of cost savings do you typically see in hospitals that implement asset management solutions?
According to our analysis, by simply reducing mobile devices by 25 percent, the average 200-bed hospital could avoid $1.3 million in capital expenditures and reduce annual service costs by $160,000. In terms of ROI, health systems that successfully adopt the enterprise asset management model can expect to reduce overall costs associated with asset management by 25 to 35 percent.
7. How can hospitals and health systems better manage their capacity and efficiency?
A great place to start is to know your clinical asset inventory and optimize utilization and governance. Organizations can also improve capacity and efficiency by applying similar methods to patients – knowing how many patients you are treating and then tracking their progress through the hospital. We’ve seen hospitals have success applying our asset tracking technology, AgileTrac, not only to clinical assets but also to patients, helping coordinate and smooth and efficient care continuum in the hospital. Tracking patients can help identify areas for improvement in terms of capacity management and efficiency.
8. Where do you see the greatest potential to improve efficiency within a hospital?
Hospitals and health systems of all sizes can reap benefits from rethinking the acquisition, management and distribution of mobile clinical assets. If inventory and utilization are better controlled, cost savings will follow.
9. How does asset management contribute to a hospital’s ability to participate in an ACO or other risk arrangement? How significant is the asset management opportunity compared to other improvement options?
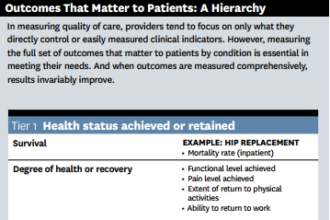
An integrated asset management approach results in outcomes and is an essential component of the ACO model. The concept of having “right asset, right condition, for the right patient” will ensure the most appropriate resources are being deployed. It is key that this is coordinated across the entire spectrum of care. Asset management is not another quick cost-out initiative. It is fundamentally changing the flow of assets, the centralized planning and on-going maintenance of assets. It is fundamentally a new way of managing resources that focuses on cost and quality outcomes.
10. Is there actually a quality impact?
Absolutely. When mobile clinical devices are immediately accessible, clean and in good working order, there is a better outcome clinically. Conditions become safer for patients and clinical staff can be more productive and focused. For example, rather than spending time searching for equipment, nurses can spend more time at the bedside with patients. When needed, the equipment is clean and in good working order. By improving these factors, there is potential to improve outcomes such as length of stay (LOS) and readmissions, which as everyone in the industry knows are two areas of growing importance as performance metrics.
11. To what extent, if any, does asset management extend beyond the 4 walls of a specific facility to include multiple hospitals or other elements of an integrated network, such as physician offices and labs?
As mentioned, oftentimes mobile devices are managed in a random, transactional manner, and this is done on a per-facility basis – meaning that each individual facility handles their own clinical assets. In larger health systems, there’s no birds-eye visibility into inventory and asset management.
Health systems can leverage asset management strategy across multiple sites with what we call a Centralized Distribution Model, where a health system coordinates and distributes assets for all of the member facilities centrally. While each member facility will have their own equipment stock, the central distribution center can allocate assets as needed across locations to meet changes in demand.